Rash and Other Problems of the Skin, Hair and Nails
Most problems of the skin, hair and nails are not as common as they once were for people living with HIV. Effective and better tolerated HIV therapy has become more widely available. However, rashes that follow the initiation of antiretroviral therapy can be common and can indicate a problematic drug sensitivity. Any rash that appears after a new drug is started should be reported to your healthcare provider or pharmacist right away. Some rashes can be serious, while others may be safe to wait out while you continue treatment.
Rash
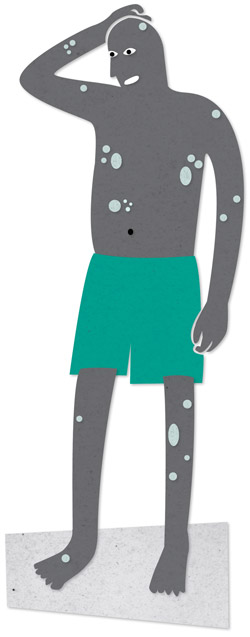
A rash is a change in the colour and texture of the skin that shows up as an outbreak of red patches or bumps. Mild rashes consist of flat, red patches appearing on a small area of the body. Moderate rashes spread over a larger area of the body and consist of flat, red patches and/or small, raised red bumps or lesions. Severe rashes are widespread and include blisters or ulcers.
Possible causes of rashes include infections (including mpox and syphilis), allergic reactions and medications. Rashes can be caused by many different medications. Sometimes the rash is mild and disappears on its own. Other times, the rash can be severe or a sign of an allergic reaction to the drug, called a hypersensitivity reaction. In these severe cases, the drug should be stopped.
Since it’s hard to know if it’s safe to continue taking a medication when a rash develops, you should report all rashes to your healthcare provider or pharmacist as soon as possible. This is especially true if the drug is known to cause severe reactions. If your healthcare provider or pharmacist is not available, go to the emergency room of the nearest hospital. If the symptoms are ignored, a lower grade rash may progress into a potentially fatal hypersensitivity reaction.
Most rashes show up within the first four to six weeks after a new drug is started. However, they can sometimes develop later. Some people develop a rash when they start taking antiretroviral therapy, most commonly if their combination contains certain protease inhibitors or non-nucleoside analogues (non-nukes). Women are more likely than men to develop a rash related to non-nukes.
For a small number of people, the protease inhibitor atazanavir (Reyataz) can cause a mild rash during the first two months, but the rash usually disappears within a few weeks of being on the drug. In rare cases, darunavir (Prezista and in Prezcobix) and fosamprenavir (Telzir) can also cause rash, and people who have an allergy to sulfa medications may be at higher risk of an allergic reaction with these medications. Occasionally, rash has also been reported with raltegravir (Isentress), maraviroc (Celsentri), and Stribild. Medicines used for treating hepatitis C can often cause rash.
At one time, serious rashes caused by hypersensitivity to the drug abacavir were somewhat common. It is now routine to screen for the risk of this reaction before abacavir is prescribed. As a result of this screening, reports of abacavir hypersensitivity reactions are rare. Rashes associated with other anti-HIV medications can also be severe, but screening for hypersensitivity to these other drugs may not be available.
Though rare, Stevens-Johnson syndrome and its more severe form, toxic epidermal necrolysis (TEN), have been associated with antiretroviral drug sensitivity. Stevens-Johnson syndrome usually begins with fever and flu-like symptoms: aches, pains, sore throat, headache and fatigue. There can also be respiratory symptoms such as difficulty breathing and a cough. Within a day or two, a burning rash develops, often over both sides of the face and upper parts of the torso, then sometimes progressing to the arms, legs, face, hands and feet. The rash can progress rapidly. It can include ulcers or blisters on mucous membranes (for example, in your mouth, on your lips or genitals), or irritation of the eyes. This reaction is life-threatening, so anyone experiencing these symptoms should go immediately to the emergency room of the nearest hospital.
Fortunately, most medication-induced skin rashes are mild to moderate, and many do not require stopping the medication. However, the only solution for severe skin rashes related to a drug is to stop taking the drug causing them. Although some drugs can be tried again at lower doses after a mild rash, this is not the case with rashes caused by abacavir or nevirapine. These drugs must never be used again.
Rashes caused by milder medications are less likely to develop into severe problems, but should still be reported to your healthcare provider. They may disappear without treatment but. ff they do not, antihistamine drugs are one treatment option. Do not take antihistamines without checking with your pharmacist or healthcare provider about the possibility of interactions with your other medications. Locally applied creams, often containing a corticosteroid, can help suppress inflammation associated with a rash, but long-term use is not recommended because of their potential to weaken the immune system when absorbed into the skin.
Less serious rashes can also be caused by a bacterial, fungal or viral infection. Infection with the germs that cause mpox or syphilis can cause a rash and, in some cases, syphilis-related rash can appear when someone starts antiretroviral therapy. A workup by an HIV-knowledgeable dermatologist may be helpful if possible, as is regular testing for syphilis in sexually active people. Diagnosing and treating any underlying infection should cause the rash to clear up quickly.
Skin and nail problems
One skin problem that can be related to antiretroviral drugs is hyperpigmentation of the palms of the hands, soles of the feet and occasionally the face. This condition is rare but can be caused by FTC, found in Truvada, Biktarvy, Descovy, Delstrigo, Genvoya, Atripla, Complera and Stribild. Hyperpigmentation related to antiretroviral medicines occurs most frequently in people with darker skin. Hyperpigmentation of the skin, tongue or nails has been linked to AZT (Retrovir, and in Combivir, Trizivir and in generic formulations).
When dryness or itchiness is part of the problem, drinking plenty of fluids, especially water if dehydration is the cause, and applying an unscented moisturizing cream or lotion can help. Some people break open a vitamin E capsule and rub the liquid, along with moisturizer, on dry skin and cracked lips. Vaseline also works well for dry, cracked lips. Zinc oxide cream, sold as a diaper rash cream or sunblock, can help eliminate some rashes.
Essential fatty acid supplements such as fish or borage oil can sometimes help with rashes and dry, itchy skin by supplying fatty acids needed for skin health and because of their natural anti-inflammatory effects. Essential fatty acid supplements can complement a multivitamin mineral supplement to provide the vitamin E, vitamin A, zinc and B vitamins necessary for good overall health, which includes good skin health.
Avoid harsh soaps that contain antibacterial chemicals and fragrances and choose hypoallergenic products. Avoid hot showers or baths. Sticking to lukewarm water will help prevent moisture loss from the skin and prevent the irritation of a rash that hot water can cause. Applying moisturizer right after bathing will lock in moisture. Oatmeal baths can also provide relief. Wearing only soft natural fabrics, especially cotton, can help. When a rash feels irritating, calamine lotion can be soothing.
Hair loss
Hair loss, also called alopecia, is a common experience in people as they age, particularly in cis men and in trans women who are not on gender-affirming hormone therapy. When hair loss is new, rapid or severe, it is considered abnormal. There are many medical treatments that can cause hair loss, including cancer drugs and some arthritis drugs.
Hair loss can also be caused by some antiretroviral medications, particularly 3TC (lamivudine, also in Combivir, Trizivir, Kivexa, Dovato, Delstrigo and in generic formulations), though this is not a common side effect. Unfortunately, no one seems to have found a perfect solution for medication-induced hair loss other than switching or discontinuing the problematic drug. Even then, in some cases, hair regrowth may be slow and incomplete.
Other causes of hair loss may include:
- malnutrition, particularly low protein intake
- thyroid problems (these can also cause hair to become coarse and brittle)
- B vitamin complex deficiency
- testosterone levels that are too high
- testosterone-based gender affirming hormone therapy
- syphilis
Androgenic steroids such as testosterone are often implicated in hair loss, particularly when high doses are used. If you are considering using testosterone, speak to your healthcare provider about its pros and cons. In general, doses that replace normal levels of testosterone, using either gels or patches, are considered best. High doses, especially by injection, should be avoided.
For some people, products that boost hair growth, such as minoxidil (Rogaine) or finasteride (Propecia), can help with hair loss. As with all medications, check to make sure there are no possible interactions with your other medications before taking such products.
