Canada is facing a drug toxicity and overdose crisis. This article provides a snapshot of data released by Health Canada on opioid- and stimulant-related harms and data from two provinces detailing a concerning trend in the nature of drug toxicity deaths in Canada. Understanding the drug toxicity and overdose crisis is essential to informing the response of governments and community-based programs that serve people who use drugs.
A note on language
The data on drug toxicity deaths from Health Canada are separated into two categories: deaths caused by opioids including fentanyl and fentanyl analogues (e.g., carfentanil) as well as non-fentanyl opioids (e.g., heroin, morphine) and deaths caused by stimulants (e.g., cocaine, methamphetamines). These categories include drug toxicity deaths (also called drug poisoning or overdose deaths) where one or more of the substances involved was either an opioid or a stimulant. The categories are not mutually exclusive as many deaths reported in one category also involved substances from other categories. For the purposes of this article, these deaths will be referred to as either opioid or stimulant toxicity deaths, when specified in the data.
However, it is important to note that the drug toxicity and overdose crisis is not being driven by particular categories or types of drugs. Rather, it is being driven by policies related to the prohibition of drugs that are meant to stop the production, transport, sale and possession of certain drugs.1,2 Prohibition creates incentives for people to produce and sell more concentrated drugs so that production and transportation costs can be reduced and profits increased,1 resulting in an unregulated drug supply that is toxic and unpredictable.3 This means that the contents and potency of unregulated drugs are often unknown, and they may contain multiple unexpected substances, which can lead to drug toxicity deaths.
Opioid toxicity deaths4
At least 21,174 people died because of opioid toxicity between 2016 and 2020. The vast majority of these deaths (e.g., 96% in 2020) were unintentional, meaning that the individuals did not die by suicide. In that time period, opioid toxicity deaths were at their highest in 2020, with 16.4 deaths per 100,000 people (compared with 6.8, 9.7, 11.0 and 9.6 deaths per 100,000 people in 2016, 2017, 2018 and 2019, respectively). In 2020, approximately 17 people in Canada died per day because of opioid toxicity. Unregulated drugs were the main cause of these deaths: 84% of opioid toxicity deaths in 2020 involved a “non-pharmaceutical opioid,” meaning an unregulated drug. In 2020, 77% of people who died because of opioid toxicity were male and the majority were aged 20 to 49 years (including all genders).
Opioid toxicity deaths are happening across the country, although western Canada (British Columbia and Alberta) have been the most affected. In 2020, the rates of opioid toxicity deaths in British Columbia and Alberta were 32.6 and 25.6 deaths per 100,000 people, respectively, far above the national average of 16.4 deaths per 100,000. Ontario (15.6 per 100,000), Saskatchewan (18.5 per 100,000) and the Yukon (14.5 per 100,000) had death rates close to the national average.
Substances involved in opioid toxicity deaths include fentanyl and fentanyl analogues (e.g., carfentanil) (82%), stimulants (52%) and other psychoactive substances (39%).* The diversity in the types of drugs involved in opioid toxicity deaths may reflect both that people may use multiple substances and the fact that the contents of the unregulated supply are often unknown.
Stimulant toxicity deaths4
Data on drug toxicity deaths that involved stimulants were reported by four to six provinces and territories between 2018 and 2020.** The vast majority of these deaths (98% in 2020) were unintentional, meaning that the individuals did not die by suicide. In 2020, Ontario had the highest known rate of stimulant toxicity deaths at 13.5 per 100,000 people, followed by Saskatchewan (11.1 per 100,000), British Columbia (7.2 per 100,0000), Nova Scotia (3.4 per 100,000), the Northwest Territories (2.2 per 100,000) and Newfoundland and Labrador (1.9 per 100,000).
Substances involved in stimulant toxicity deaths include cocaine (68%), methamphetamines (47%), opioids (84%) and other psychoactive substances (21%). The diversity in the types of drugs involved in stimulant toxicity deaths may reflect both the fact that people may use multiple substances and the fact that the contents of the unregulated supply are often unknown.
The COVID-19 pandemic
After the implementation of measures to prevent the spread of COVID-19 in Canada (e.g., physical distancing), there were 5,148 opioid toxicity deaths (April to December 2020), which is an 89% increase from the same period in 2019.4 The increase in drug toxicity deaths during the pandemic may be an unintended consequence of measures taken to reduce community transmission of the virus that causes COVID-19. These include increased toxicity and unpredictability of the illicit drug supply due to border closures,5,6 reduced availability and accessibility of harm reduction services, and increased feelings of isolation, stress and anxiety, among many other factors.4
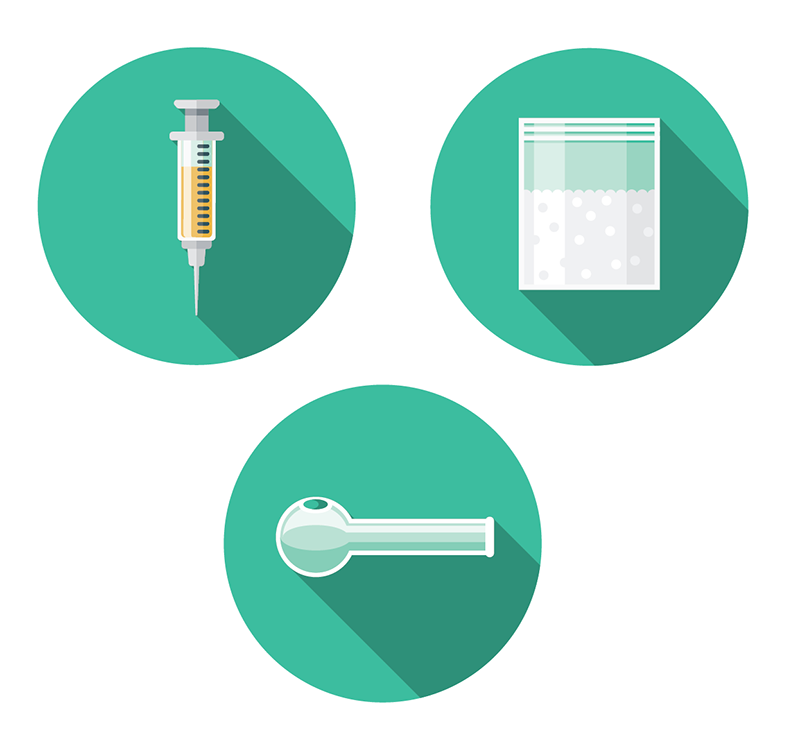
Mode of drug consumption
Provincial data from select provinces indicates that smoking drugs is leading to a higher proportion of drug toxicity deaths than injecting drugs. Example data from British Columbia and Ontario*** are presented below. This data is largely compiled by observing the equipment found at the scene of an overdose death.#
In British Columbia, smoking^ has been the most common mode of drug consumption resulting in death since 2017. Drug toxicity deaths from smoking increased from 28% of total drug toxicity deaths in 2016 to 40% in 2019. Drug toxicity deaths from injecting fell from 37% of total drug toxicity deaths in 2016 to 25% in 2019. This indicates that drug toxicity deaths with evidence of drug smoking are more common than those with evidence of injecting. Intranasal and oral drug consumption were associated with 20% and 10% of drug toxicity deaths in 2019, respectively; in 21% of cases the mode of consumption was unknown.7
In Ontario, data indicate that smoking has been the leading cause of drug toxicity deaths during the COVID-19 pandemic. Modes of drug consumption resulting in death were compared between a period before the pandemic (March 16 to December 21, 2019) and a period during the pandemic (March 16 to December 31, 2020). The proportion of drug toxicity deaths from smoking increased significantly from 23% (pre-pandemic) to 34% (pandemic). During the same time frame, the proportion of drug toxicity deaths that were a result of injecting opioids decreased significantly from 18% (pre-pandemic) to 14% (pandemic).8
What does this mean for service providers?
People in Canada are dying because of drug toxicity at unprecedented rates, and limited data indicate that smoking drugs is associated with a greater proportion of drug toxicity deaths than injecting drugs. In the past, there was an assumption that injecting drugs carried a higher risk of harm as it was tied to the transmission of blood-borne infections such as HIV and hepatitis C. However, these recent data highlight the harm associated with smoking drugs and the need for programs to consider whether and how their services are meeting the needs of people who smoke drugs.
A variety of harm reduction approaches need to be expanded to prevent drug toxicity deaths in Canada, including supervised consumption sites and overdose prevention sites that allow for different modes of drug consumption (e.g., injection, smoking), the increased provision of smoking supplies, drug checking initiatives, safe supply, naloxone distribution and educational initiatives.
Supervised consumption sites and overdose prevention sites where people can smoke drugs in the presence of workers trained in overdose response are urgently needed; they are currently uncommon in Canada. In the absence of facilities purpose built for smoking indoors, some overdose prevention sites or supervised consumption sites have provided people who smoke drugs with access to outdoor spaces where they can be monitored for signs of drug toxicity.
The increasing number of deaths caused by the unregulated drug supply indicates the potential importance of drug checking initiatives. These services can help monitor the local drug supply and allow harm reduction organizations and people who use drugs to increase their knowledge and awareness of the changing contents and potency of illicit drugs. This knowledge can help inform services, education and other harm reduction measures.
There is also a need to provide legal and regulated alternatives to the illicit drug supply for people who use drugs. As these interventions, called safe supply, are being developed, evaluated and expanded across parts of Canada, it is important that they consider and include people who smoke drugs and people who use stimulants and other drugs to ensure their needs are being met.
In terms of broader efforts to support the health of people who use drugs, as more individuals smoke their drugs the distribution of harm reduction equipment should include supplies appropriate for smoking (e.g., straight stems, bowl pipes, push sticks, brass screens, mouthpieces, foil). These supplies are proven to help reduce infections such as HIV and hepatitis C among people who use drugs and to prevent burns, cuts and other harms caused by smoking with homemade equipment. Organizations providing services to people who use drugs should be aware of the unpredictable nature of the unregulated drug supply and be prepared to provide education and services accordingly (e.g., the distribution of naloxone).
Data limitations
The data presented in this article are based on information reported by Health Canada and provincial and territorial governments on drug toxicity deaths and have limitations. First, no number can capture the unique stories, qualities, challenges and strengths of each person who has been killed by prohibition or the burden of grief and loss that accompanies their deaths. Second, provinces and territories differ in how they investigate and classify deaths and conduct toxicology testing, which may affect the ability to compare data between provinces and territories. Third, data on opioid toxicity deaths and stimulant toxicity deaths are not mutually exclusive, as people may use multiple substances and the contents of the illicit supply are often unknown.
Related resources
Best Practice Recommendations for Canadian Harm Reduction Programs
Responding to an Opioid Overdose, Responding to Stimulant Overuse and Overdose
References
- Beletsky L, Davis CS. Today’s fentanyl crisis: Prohibition’s Iron Law, revisited. International Journal of Drug Policy. 2017;46:156-9.
- Office of the Provincial Health Officer. Stopping the harm: decriminalization of people who use drugs in BC. Victoria (BC): Office of the Provincial Health Officer; 2019. Available from: https://www2.gov.bc.ca/assets/gov/health/about-bc-s-health-care-system/office-of-the-provincial-health-officer/reports-publications/special-reports/stopping-the-harm-report.pdf
- Crabtree A, Lostchuck E, Chong M et al. Toxicology and prescribed medication histories among people experiencing fatal illicit drug overdose in British Columbia, Canada. Canadian Medical Association Journal. 2020;192:967-72.
- Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and stimulant-related harms in Canada. Ottawa: Public Health Agency of Canada; March 2021. Available from: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants
- BC Coroners Service. Illicit drug toxicity deaths in BC: January 1st, 2010 - January 31st, 2020. Victoria (BC): Ministry of Public Safety and Solicitor General; 2020. Available from: https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/statistical/illicit-drug.pdf
- Bridges A. Drug users, advocates weigh in on why Sask. overdose deaths are at record high. CBC News. 2020 Sept. 14. Available from: https://www.cbc.ca/news/canada/saskatoon/overdose-deaths-record-interviews-addicts-saskatchewan-1.5723019
- Ministry of Public Health & Solicitor General. Illicit drug toxicity deaths in BC. Knowledge update: mode of consumption. June 2020. Available from: https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/statistical/mode-of-consumption.pdf
- Gomes T, Murray R, Kolla G et al, on behalf of the Ontario Drug Policy Research Network, Office of the Chief Coroner for Ontario and Ontario Agency for Health Protection and Promotion (Public Health Ontario). Changing circumstances surrounding opioid-related deaths in Ontario during the COVID-19 pandemic. Toronto, ON: Ontario Drug Policy Research Network; 2021. Available from: https://www.publichealthontario.ca/-/media/documents/c/2021/changing-circumstances-surrounding-opioid-related-deaths.pdf?la=en
* The term “other psychoactive substances” refers to alcohol, benzodiazepines, gabapentinoids and/or other psychedelics and dissociatives.
** National numbers are not available because of limited data.
*** Data may be available in other regions; check with local provincial /territorial governments to confirm.
# Equipment can include supplies for injecting (e.g., needle/syringe) and/or supplies for smoking (e.g., pipes, foil). Limitations of data collection include the fact that the presence of equipment may reflect previous drug use and/or use of drugs by someone else.
^ BC uses the term smoking and Ontario uses the term inhalation. Both provinces are referring to situations where evidence of smoking drugs (e.g., equipment for the smoking of drugs such as pipes or foils) was found. For simplicity this article uses the term smoking.
About the author(s)
Amanda Giacomazzo is CATIE’s manager of community programming. She has a master’s degree in health science with specialised training in health services and policy research and previously worked in knowledge translation and public health at the provincial level.
Magnus Nowell is CATIE’s knowledge specialist in harm reduction. Magnus has previously worked in harm reduction research, community organizing and housing. He has a master’s degree in health promotion.
Laurel Challacombe holds a masters degree in epidemiology and is currently director, HIV knowledge exchange and evaluation at CATIE. Laurel has worked in the field of HIV for more than 10 years and has held various positions in both provincial and regional organizations, working in research and knowledge transfer and exchange.