- Ontario researchers studied syphilis among street-involved people in small towns
- They found higher rates among women and people who use drugs
- Syphilis rates were highest among those who had an intersection of risk factors
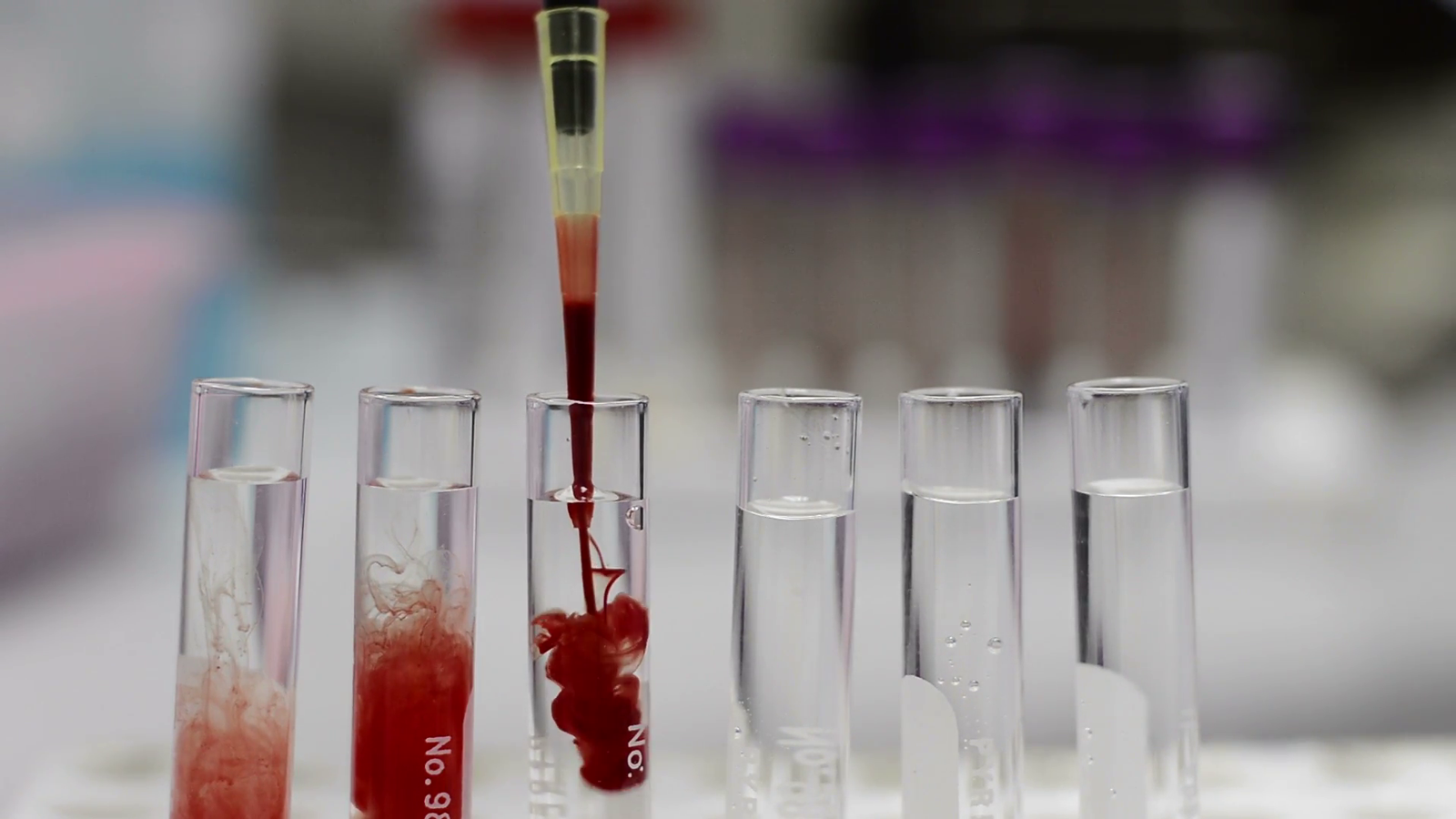
Diagnoses of sexually transmitted infections (STIs) have been increasing over the past 20 years, and now there is an epidemic of syphilis across Canada. The initial symptoms of syphilis—a sore or chancre on or inside the genitals, mouth or other parts of the body—may be painless or go unnoticed. The germs that cause syphilis (called treponemes) quickly spread from the site of first contact. These germs can attack nerves, eventually causing problems in the ears (hearing loss) and eyes (loss of vision). What’s more, if left untreated, over time syphilis can cause injury to vital organs, including the brain, bones, heart and circulatory system, liver and kidneys. Syphilis during pregnancy can harm the fetus and baby (congenital syphilis). Symptoms of syphilis can mimic many other diseases; however, syphilis can be easily diagnosed with a simple blood test. Most people can recover with a single course of antibiotic therapy.
In Ontario
According to a team of researchers across Ontario, diagnoses of infectious syphilis quadrupled between 2013 and 2023. They stated that although historically syphilis has disproportionately affected men—particularly gay, bisexual and other men who have sex with men (gbMSM)—the surge of syphilis in Ontario has resulted in women of reproductive age being the “fastest growing at-risk group.” What’s more, they stated that this shift in populations affected by syphilis is even “more pronounced in rural and smaller urban areas across Ontario.”
The research team added that “much of the existing epidemiological research on syphilis among street-involved populations has focused on clinical cohorts in major urban centres.” So, the team stated that they decided to conduct a study on syphilis across “small urban, rural, and remote public health units in Ontario.”
Study details
Researchers collected data from an ongoing study called (SPRITE) in which public health nurses used a rapid point-of-care STI test called the INSTI Multiplex HIV-1, HIV-2 and syphilis antibody test. People who tested positive for syphilis with this test were offered immediate treatment. People who tested positive for HIV with the test had this infection confirmed with standard laboratory testing. As the study was focused on syphilis screening, researchers did not provide details about HIV care, but presumably people who tested positive for the virus would be referred for care.
The study nurses visited a variety of locations in small urban centres and rural areas to offer rapid syphilis testing, including the following:
- supervised consumption sites
- homeless shelters
- encampments
- mobile harm reduction units
The researchers had what they called an inclusive definition of “street-involved,” which accounted for “both varying degrees of homelessness and a wide range of risk factors, including drug use and survival sex.” Thus, the study engaged people who were not necessarily homeless but “who were exposed to and experiencing the physical, mental, emotional, and social risks of street [life].”
Data, collected between June 2023 and November 2024, focused on 630 people whose average profile was as follows:
- 58% cisgender men and 42% cisgender women
- age – 38 years
- 62% had unstable housing
- 7% were gbMSM
- nearly 40% had multiple and/or anonymous sexual partners
- 11% engaged in current or past sex work
Drug use
Researchers collected data on the type of drugs used after April 26, 2024, and 426 people disclosed that they used drugs. The most commonly used drugs were crystal methamphetamine (47%), fentanyl (45%), and crack and/or cocaine (44%). Overall, 44% of people who disclosed drug use revealed that they used more than one type of drug.
Focus on syphilis
Researchers found that nearly 8% of participants tested positive for syphilis.
Positive test results for syphilis were higher among women (10%) compared to men (6%). Rates of positive syphilis tests among women varied according to age group, as follows:
- 40 to 49 years – 18% positive
- 20 to 29 years – 12% positive
- 30 to 39 years – 8% positive
Women who had unstable housing were more likely to have a positive syphilis test result (12%) than men with unstable housing (8%). A similar difference was seen between women and men who used drugs.
Risk factors
According to the researchers, “individuals reporting sexual risk factors had higher [rates of positive syphilis test results] compared with those without such risk factors,” as follows:
- a history of sex work – 20% tested positive
- anonymous sexual partners – 16% tested positive
- multiple sex partners – 12% tested positive
- people who disclosed injecting drugs – 10%
- people who used drugs – 9%
Among people who used drugs, those who disclosed their use of crystal methamphetamine were most likely to have a positive test result for syphilis.
The researchers noted an intersection of risk factors—nearly 20% of participants who had sexual risk factors also used drugs and had unstable housing. People who reported all three risk factors were at heightened risk for having syphilis.
Bear in mind
The Ontario study has uncovered high rates of syphilis among street-involved people in small urban centres and rural Ontario. The researchers stated that “women, people who used drugs and those with sexual risk factors” generally had the highest rate of positive test results.
Although men account for most cases of syphilis in many studies of this STI in Canada and other high-income countries, women are increasingly a significant population with syphilis. The present study confirms this trend.
The researchers advanced the possibility that rates of injection drug use, particularly with methamphetamine, may have increased among women. A U.S. study found that between 2013 and 2017 rates of injecting drugs, including methamphetamine, increased among women who were subsequently diagnosed with syphilis. A study in Canada has found that use of methamphetamine is on the rise.
The researchers caution that the risk factors they have identified do not operate in isolation. Rather, such risk factors occur within “broader social, structural and historical contexts.”
The study did not collect information on mental health and sexual networks—these have been identified as risk factors for syphilis in previous studies.
The present study has identified overlapping risk factors and an undue burden of syphilis among women. The researchers stated that their study underscores “the urgent need for targeted, equity-oriented outreach models.” Furthermore, they added that their results can “inform clinical practice by guiding risk-based screening strategies and supporting policy development to scale integrated, community-based STI care to reduce transmission and address structural health inequities.”
—Sean R. Hosein
Resources
Sexually transmitted and blood-borne infections: Guides for health professionals – Public Health Agency of Canada
STI-associated syndromes guide: Syndromic management – Public Health Agency of Canada
CATIE statement on the use of doxyPEP to prevent syphilis
Winnipeg researchers warn about rising cases of syphilis-related stillbirths – CATIE News
Views from the front lines: Congenital syphilis – CATIE
Congenital syphilis – NCCID
Early access to syphilis screening and treatment needed to prevent stillbirths – CATIE News
Rapid combined syphilis-HIV testing found accurate and useful in an Alberta study – CATIE News
Alberta study underscores the importance of syphilis testing in people who use stimulants – CATIE News
New HIV infections in Manitoba intersect with housing and methamphetamine use – CATIE News
Understanding the impact of the antibiotic doxycycline on the sexual well-being of users – CATIE News
REFERENCES:
- Mackrell L, Antoun JP, Carter M, et al. Intersecting risk factors associated with high syphilis seroprevalence among a street-involved population in Canada. Open Forum Infectious Diseases. 2025 Aug 7;12(8): ofaf472.
- Chevalier FJ, Bacon O, Johnson KA, et al. Syphilis: A Review. JAMA. 2025; in press.