What is the program?
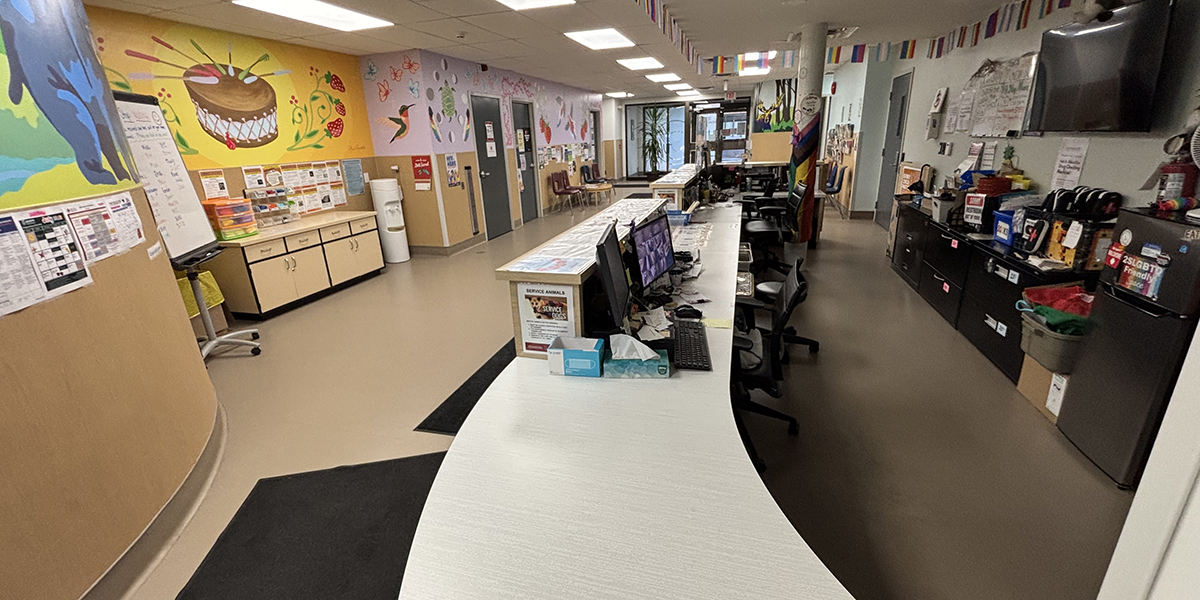
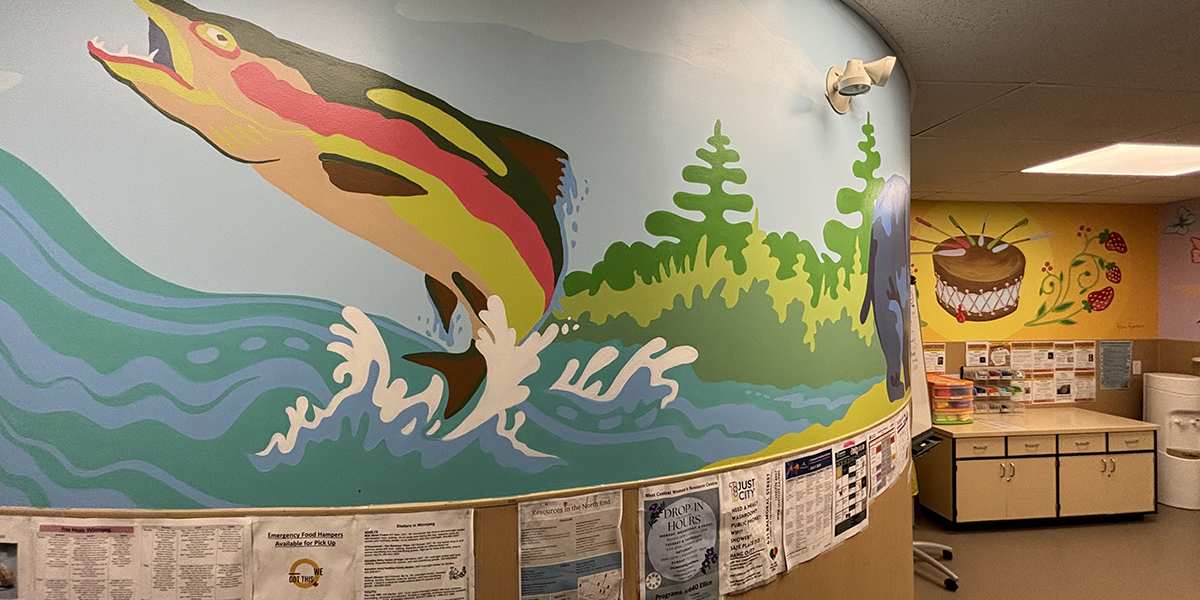
The Pit Stop is a lower barrier, harm reduction drop-in centre operated by Nine Circles Community Health Centre (NCCHC) in Winnipeg’s West Broadway neighbourhood. The Pit Stop provides a non-judgmental space for people who use drugs, people living with and at risk of HIV, people who are experiencing houselessness and people who face barriers to accessing healthcare. The program offers access to harm reduction supplies, testing for sexually transmitted and blood-borne infections (STBBIs), drug checking services, take-home naloxone kits, on-site nursing, basic hygiene products and cultural support.
NCCHC is a community health centre specializing in HIV prevention and care that serves communities affected by HIV, poverty and social exclusion. The Pit Stop reflects NCCHC’s mission to provide lower barrier, culturally safe care while eliminating stigma and advancing health equity.
Why was the program developed?
The Pit Stop was developed in response to Manitoba’s intersecting crises of HIV transmission and drug toxicity deaths. Manitoba experienced a 240% increase in new HIV diagnoses from 2018 to 2024, with transmission primarily affecting Indigenous women, people who use drugs, people who are experiencing houselessness and people living in extreme poverty. This alarming trend, paired with a rise in toxic drug overdose fatalities, led the Manitoba HIV Program to issue a call to action, emphasizing the need for prevention and expanded harm reduction services for people at risk of HIV and other STBBIs and people at risk of overdose. In response, the Pit Stop was created to provide HIV prevention and harm reduction services to address service gaps by focusing on education, wellness and destigmatized care for marginalized populations.
The Pit Stop has three primary goals:
- prevention of and education about HIV, other STBBIs and drug-related harms (e.g., overdose, death)
- testing and early diagnosis to connect people to care
- wellness through holistic, non-judgmental and culturally appropriate support
How does the program work?
The Pit Stop services include the distribution of safer drug use and safer sex supplies, drop-in nursing services (e.g., STBBI testing, wound care), harm reduction education and overdose prevention, drug checking, systems navigation and connections to community services, education opportunities and other social supports, and access to a safer public bathroom. On average, over 150 people access the Pit Stop every day — a number that has continued to rise steadily since it first opened in 2020.
The Pit Stop is open Monday to Friday from 9:00 a.m. to 4:55 p.m. Community members can drop in for 10 to 15 minutes to access harm reduction supplies, speak with staff and be connected to additional care services (e.g., mental health services). The program is generally open to adults of all ages; it primarily serves people living with and at risk of HIV, people who use drugs, people who are experiencing houselessness and street-involved, Indigenous people, 2SLGBTQIA+ community members, immigrants and newcomers and people experiencing complex poverty. The program is staffed by an integrated, multidisciplinary team that includes community hosts (CHs), health education facilitators (HEFs), a nurse and a cultural support worker.
When community members arrive at the Pit Stop entrance, they are greeted by CHs who provide a welcoming, trauma-informed first point of contact. Seeing a familiar face at the entrance every day is an important part of relationship- and trust-building between community members and staff. Harm reduction supplies and drug checking services are provided by CHs and HEFs. If someone is looking for HIV and other STBBI testing and is eligible for the service (i.e., people at risk of HIV and other STBBIs, people with new HIV diagnoses), HEFs connect them to the on-site nurse, who completes an assessment and the testing process as well as arranges for follow-up care as necessary. Depending on a person’s needs and requests, HEFs can also redirect people to a variety of other services available in the community.
The steady flow of community members through the front area means that staff spend considerable time focusing on connecting with individuals and responding to their requests. In collaboration with the CHs, HEFs monitor the front entrance and the safer public washroom open to people accessing the Pit Stop. To ensure safety and security, the CHs and HEFs monitor individual behaviours, proactively assess and manage potential issues, and engage in on-site crisis response if needed. Staff assess community members’ eligibility for the Pit Stop and other NCCHC programs and services by engaging in conversations with them and helping to direct them to services. If a person does not fit the eligibility criteria of the Pit Stop and does not already access services at NCCHC, HEFs and CHs redirect them to other services available in the community that can better address their specific needs.

Supply distribution, education and overdose prevention
Along with the distribution of safer drug use supplies and supplies for safer sex (e.g., condoms), the Pit Stop provides free take-home naloxone kits and overdose response training. To uphold privacy and confidentiality, the Pit Stop does not require individuals accessing harm reduction supplies to provide personal information. If follow-up is required, people are asked to provide contact information such as a phone number or the contact information of another local organization or service provider they frequently access.
HEFs offer one-on-one education about overdose prevention, safer drug use techniques and how to respond to emergencies. HEFs and CHs are all trained in overdose response and help ensure timely intervention when necessary. A safer public bathroom policy with timed access, routine checks at the door and staff monitoring enhances safety on-site.
Drug checking
The Pit Stop offers free, legal and confidential drug checking services using a Fourier-transform infrared (FTIR) spectrometer. This service allows people to test their drug samples and receive real-time information about the contents. Drug testing strips are also used to help detect substances, particularly for very small sample sizes and substances below threshold limits. People can have their drugs checked by HEFs at the Pit Stop in a private office space on Tuesdays, Wednesdays and Thursdays between 10:00 a.m. and 4:00 p.m. Depending on service demand and the length of their interaction with staff, people generally receive their drug checking results within 15 to 30 minutes.
Drug checking empowers people to make safer and more informed decisions, reduces risk of overdose and contributes to public health surveillance. Results are shared with community partners like Street Connections and Sunshine House to issue community drug alerts and track drug supply trends. These drug checking services offer a critical entry point for deeper engagement, education and support.
Other on-site services and connections to care
In addition to harm reduction supply distribution and education and drug checking, the Pit Stop provides on-site nursing, cultural support, referrals to primary care and mental health support, access to basic wellness supplies and opportunities for recreation.
Drop-in nursing: The on-site nurse offers same-day wound care, STBBI testing, pregnancy tests, HIV care and mental health and substance use assessments and service referrals. These nursing services are only accessible to people actively using the Pit Stop who are at risk of HIV and other STBBIs, people with a new HIV diagnosis and people looking to engage in HIV care. The nursing office is located in the Pit Stop space and the on-site nurse is generally available during the program opening hours to ensure consistency and accessibility.
Cultural and spiritual supports: The cultural support worker providers culturally relevant services, lower barrier access to medicines, smudging and beading, as well as cultural and Indigenous healing and wellness supports. The cultural support worker is also available to people accessing primary care in the NCCHC clinic to provide accompaniment, support and comfort while they are accessing healthcare.
Connections to primary care and mental health supports: HEFs help facilitate access to the comprehensive NCCHC’s integrated primary healthcare team for people living with HIV. In-house service providers include doctors, nurses, a pharmacist, a dietitian, outreach and social workers, mental health therapists and an occupational therapist. If a person’s specific needs cannot be met by the in-house NCCHC team, HEFs connect them to local community-based organizations, primary care and other programs that can better address their needs, and Pit Stop staff can provide systems navigation and accompaniment to appointments in the community (e.g., hospital, social worker, organizational partners).
Access to basic wellness supplies: On the basis of supply availability, HEFs facilitate access to snacks, drinks, seasonal clothing, camping gear, footwear and hygiene products (e.g., soap, menstrual products).
Opportunities for recreation and connection: In collaboration with other staff at NCCHC, the Pit Stop staff help organize activities that foster community and connection among people. This includes Indigenous cultural programming (e.g., ribbon skirt and shirt making, beading, drumming, sewing and mending), informal social circle drop-in sessions, group-specific sharing sessions (e.g., women and gender diverse group), as well as meditation and mindfulness workshops (e.g., “just breathe” drop-in).
Workshops, information sessions and other social supports: The team works collaboratively with external service providers to help people secure housing, access food hampers, apply for identification (ID) and connect with other social supports. The program also hosts partner organizations to provide workshops on topics such as housing and tenant support and pest management; offer ID clinics; and help with applications for social benefits and Child and Family Services settlements (e.g., Citizens’ Bridge, Sara Riel Housing, West Broadway Community Organization, Oyate Tipi Cumini Yape, CancerCare Manitoba).
Harm Reduction Peer Advisory group
The Harm Reduction Peer Advisory (HRPA) group provides leadership and insight from people with living and lived experience of substance use to guide the design, delivery and evaluation of the Pit Stop’s services. Members of the committee are people who access the Pit Stop’s services and help ensure that peer perspectives are meaningfully integrated across the program. Meeting approximately once a month, the group collaborates with the multidisciplinary NCCHC Health Promotion Team on specific projects (e.g., anti-stigma project, third space project), provides input on program structures and policy changes and helps develop feedback surveys. Some members also co-facilitate workshops and education sessions for people who access the Pit Stop. HRPA members are compensated with hourly cash honorariums, food, bus tickets and access to additional professional development opportunities.
Staff hiring, training and funding
The Pit Stop is supported by an integrated, multidisciplinary team that includes CHs, HEFs, a nurse and a cultural support worker. As part of their role, staff receive continuous training (e.g., non-violent crisis intervention, trauma-informed approaches, de-escalation techniques, drug checking) to maintain and strengthen their capacity for crisis response. Staff are also encouraged to participate in a variety of professional development activities through seminars, webinars, conferences and community engagement opportunities (e.g., networking, workshops).
The Front-Area Safety Team (FAST) is a multidisciplinary group that supports safety planning at the Pit Stop and all other NCCHC facilities. The FAST group consists of NCCHC managers, building operators, social workers and the Health Promotion Team, which includes Pit Stop HEFs. On a monthly basis, they meet to discuss building design, safety protocols and case-by-case management.
Many staff and volunteers have living and lived experience of substance use and are supported and trained to provide inclusive care. Funding increases and provincial policy support have allowed for staff expansion and service enhancement over time.
Required resources
- HEFs, CHs, nurse and cultural support worker
- Harm reduction supplies (e.g., syringes, bubble pipes, stems, naloxone kits, condoms, HIV self-tests)
- Drug checking equipment and training (e.g., FTIR spectrometer)
- Space for cultural support and connection (e.g., round room), as well as culturally relevant supplies (e.g., smudge kits, medicines, beading materials)
- Snacks, drinks and seasonal gear (e.g., tents, sleeping mats, warm clothing, shoes)
- Basic hygiene supplies (e.g., soap, menstrual products)
- Partnerships with local community-based organizations and programs to facilitate workshops and connections to other care services
- Transparent codes of conduct and policies for safety and emergency medical response
- Administrative support to facilitate evaluation
- Physical design centred on safety (e.g., having good sight lines, adequate lighting, single entrance, safer washroom design)
- Honorariums and bus tickets for HRPA members
Evaluation
Between 2020–2021 and 2024–2025, the Pit Stop saw major growth:
- Visits increased from 7,153 to 29,154
- Syringe distribution rose from 174,340 to 240,620
- Safer smoking kit distribution increased from 2,717 to 8,508
- Naloxone kits distributed: 6,331 (data only available for 2024–2025)
An external evaluation conducted in 2023 reviewed administrative data, surveys of Pit Stop staff and community members who access the program, and one-on-one follow-up interviews with the Pit Stop staff. Key findings highlighted that:
- 87% of people listed harm reduction supplies as their main reason for accessing the Pit Stop
- 96% of people reported an increased ability to use drugs more safely
- 97% of staff and volunteers agreed that the Pit Stop increased access to harm reduction supplies
- 87% of staff and volunteers agreed that the Pit Stop increased knowledge about harm reduction
- 90% of staff and volunteers agreed that services at the Pit Stop resulted in increased uptake of harm reduction practices
The nurse tested 81 individuals for an STBBI (68 for the first time), diagnosed three new cases of HIV and connected all three people to care (results for other STBBI tests not available). Finally, the external evaluation found that overall, emergency incidents decreased because of effective frontline conflict and crisis management.
Staff at the Pit Stop shared the following:
“Pit Stop is very important and needs to be very well resourced. It’s an opportunity to deliver healthcare in a unique way for a community of people living with HIV who do not have access right now in a way that they need it — really flexible, low barrier and paired with harm reduction services.” (evaluation interview respondent)
“Adopting HR [harm reduction] practices is a big [outcome of the Pit Stop]. We try to connect with people on a personal level … give them tips they can take or not. I find that people are very open to receiving it.” (evaluation interview respondent)
Challenges
- Because of high and increasing program attendance and eligibility criteria for some services (e.g., drop-in nursing), opportunities for consistent, meaningful engagement, education and connections to care are limited.
- Balancing lower barrier, non-intrusive access with more intensive STBBI prevention and education is difficult for staff with limited time.
- Follow-up can be challenging when individuals with a previous connection to the Pit Stop become disengaged from care and lack access to a phone and/or are experiencing houselessness or precarious housing.
- People are sometimes turned away because services are unavailable or there are staffing gaps, often related to reproductive health care, wound care and other social supports.
- Service coverage is limited and there is a need for more support in rural and remote areas.
- The drug checking service is limited by technology and access hours.
- Intersecting crises of extreme poverty, houselessness, housing affordability and availability, the toxic drug crisis and rising HIV cases complicate service delivery because people are navigating multiple issues and need help accessing numerous and limited services in the community.
Lessons learned
- Consistency and safety are foundational — familiar staff, supportive management, clear expectations, transparency and strong policies foster trust, connection and reliability.
- Peer involvement is critical — people with living and lived experience shape programming and support cultural safety.
- Integration and visibility — access to health education, nursing and cultural support services directly in the Pit Stop space is essential to engaging people on the spot in education, prevention and care.
- Small interactions matter — brief contact can still lead to safer use and improved health and social outcomes.
- Lower barrier models work — the Pit Stop has improved safety, reduced stigma and created a strong sense of community and belonging.
- Investment pays off — resources directed at frontline harm reduction result in greater community engagement and increase access to care.
- Relationships are healthcare — meeting people where they’re at is essential to prevention, testing and wellness.
Program materials
- Nine Circles Community Health Centre Annual Report 2024-2025
- The Pit Stop (Harm Reduction)
- The Pit Stop: Community Health Education and Drug Checking
- NCCHC Drug Testing Machine: Frequently Asked Questions
- Manitoba HIV Program
- HIV is Here, and So is Support
- Sex Friendly Manitoba
- Sex, Drugs & Bingo
- Community Safety Host
Contact information
Health Education Facilitators
The Pit Stop
Nine Circles Community Health Centre
705 Broadway
Winnipeg, Manitoba
R3G 0X2
204-940-6000
ninecircles@ninecircles.ca