Introduction

Bridging Western and First Nation treatment approaches
In the heart of Vancouver’s Downtown Eastside, the Towards Aboriginal Health and Healing (TAHAH) program offers a network of supports to First Nation people living with HIV who are navigating a myriad of health and social burdens, including street involvement, poverty and acute use of multiple substances. A common thread woven into the clients’ personal stories is distrust of mainstream institutions that provide care, because of personal, historical and institutional traumas.
TAHAH is an HIV treatment, care and support initiative that aims to support clients’ stability and improve their overall health through clinical and outreach work. It uses Western medicine and traditional and contemporary First Nation knowledge and practices. First Nation peer community advocates and an Elder work within an interdisciplinary team including nurses and an intensive case manager to provide extensive support.
When you walk through the doors at the Vancouver Native Health Society (VNHS), where TAHAH is housed, you step into a world where First Nation cultures are visible and tangible. Despite the many people moving about in a buzz of activity, clients and staff are very friendly and greet everyone who enters. You will see multiple things occurring simultaneously, from casual conversations to crisis interventions to triage. Food is being offered and shared. Phones ring. You will also get the sense that much more is happening behind the scenes.
TAHAH staff will tell you that as clients connect with healing, all of its members and indeed the fabric of the community are strengthened.
The TAHAH program, with the support of VNHS, AIDS Vancouver and the Seek and Treat for Optimal Prevention of HIV/AIDS (STOP) initiative, is designed to foster authentic and therapeutic connections with HIV-positive First Nation people who are falling through the cracks in the healthcare system. These connections are considered the essential path to increased health and social well-being.
What is the Program?
Towards Aboriginal Health and Healing (TAHAH) is a clinical and outreach-based program that supports clients to stabilize and improve their overall health. For clients who are not on HIV treatment or able to adhere to it, the program helps them to stabilize factors that affect their ability to consider, start and adhere to treatment. This support, treatment and care program works with extremely marginalized First Nation people living with HIV in the Downtown Eastside of Vancouver. It is based at the Vancouver Native Health Society (VNHS), an organization that delivers comprehensive medical, counselling and social services to Vancouver’s Downtown Eastside community.
Typically, TAHAH clients are referred to the program by a physician, nurse or support worker from the community or through another VNHS program, the Positive Outlook Program. All TAHAH clients are referred because they need a higher level of support than they are currently receiving to achieve and maintain stability in their lives. For example, a client who visits VNHS daily for lunch served in the Positive Outlook Program may be referred to TAHAH because they are not on antiretroviral therapy. Another client may be on antiretroviral therapy but may be referred to TAHAH because they are unable to maintain their methadone treatment.
The TAHAH program, which has an active case load of 25 to 30 clients, is carried out by a multidisciplinary team of individuals who work together very closely. The team includes nurses, an Elder, an intensive case manager and peer community health advocates. The peers are trained First Nation people living with HIV from the community, who help engage and support TAHAH clients.
Once engaged, clients can access a range of healthcare and social supports through TAHAH. Family doctors and infectious disease specialists provide services in clinic, and TAHAH’s nurses and case manager serve clients in clinic and through outreach.
When clients have shown that they can manage their own HIV care and have achieved stability in several other aspects of their lives, they may “graduate” from TAHAH. People will also graduate when they move out of the Downtown eastside and no longer access services at VNHS. The program typically graduates one or two people per year.
Philosophy of care
The TAHAH program employs a holistic model of care that integrates care for the physical, spiritual/traditional, mental/emotional and social needs of their clients and staff. Program staff do not simply provide basic medical care and HIV treatment; they also recognize the power of music and art; the need for food, housing and sleep; and the need for comprehensive, individualized addiction treatment when treating HIV and other chronic and debilitating diseases.
Integrating First Nation and Western care
TAHAH works from an Indigenous context, which means that Western and First Nation knowledge systems are seen to be of equal value—and that both are viewed as necessary components of healthcare delivery to First Nation people. “The challenge,” says a VNHS physician, “is for Western practitioners to create and ensure the professional space required for Aboriginal cultural knowledge and practices.”
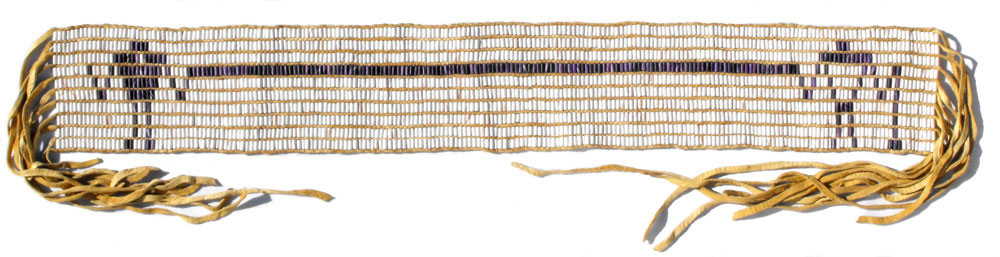
At VNHS, which houses TAHAH, the strengths offered by the two forms of knowledge are recognized, leading to an atmosphere of mutual respect. The senior physician at VNHS, Dr. David Tu, describes the relationship between Western and First Nation traditions at VNHS by recalling the earliest treaties recorded on Wampum belts. The Two Row belt seen below depicts the relationship between First Nations and the settlers: they are like two canoes sharing a river, each with its own way of doing things, yet equal brothers.
http://www.wampumchronicles.com/
VNHS established this mutual respect through years of relationship building across these two communities and the use of the medicine wheel in all programs and services. The medicine wheel teaches about respect and inclusion. TAHAH engages staff and volunteers who value both forms of knowledge and who are committed to being guided by the medicine wheel.
Why Was the Program Developed?
Two paradigm shifts at VNHS led to the creation of the TAHAH program. By 2005, improvements in HIV treatment were enabling people living with HIV to live longer, healthier lives. As a result, HIV care at VNHS around this time was shifting from an infectious disease model to a chronic disease management model. The chronic disease management model allowed the VNHS team to focus on longer term outcomes for client care, including patient self-management. This shift also led to VNHS developing programs that aimed to address the barriers that some people face in accessing HIV treatment.
While this approach resulted in significant improvements in HIV care for First Nation clients at VNHS, it was apparent that some First Nation people living with HIV in the community were still falling through the cracks and not receiving adequate healthcare. The low-barrier, standardized model of health care offered at the clinic at that time did not work for the complex health needs and social circumstances of these individuals.
At the same time (2005-7), VNHS was participating in a research project that involved training four First Nation people living with HIV as community-based researchers. The four peers completed a year-long intensive training program with Simon Fraser University and developed a range of skills including in-depth peer support. These individuals were clients of the Positive Outlook Program at VNHS, and through this peer work, started to become more embedded in the organization.
The insights gained at VNHS through the adoption of a chronic disease management model and the integration of the peer community advocates into the organization informed the TAHAH program model. To successfully engage the individuals in the community who needed extensive support to stabilize their lives so that they could ultimately access standardized care, an intensive case management approach was developed that included the trained peers as core program staff.
The goals developed for the TAHAH program aligned with the goals of the STOP project, including improving access to HIV care and treatment. In 2011, the TAHAH program began to operate with funding support offered by STOP.
How Does the Program Work?
Location
The TAHAH program is located at the Vancouver Native Health Society (VNHS), one of the busiest clinics in Vancouver’s Downtown Eastside. Established in 1991, the clinic embraces a harm reduction philosophy in the treatment and support of its clients. In addition to providing a broad range of healthcare services, VNHS offers several harm reduction services: methadone maintenance, addictions counselling, diabetes awareness, Sheway (providing assistance to women and their infants struggling with issues of addictions) and the Positive Outlook Program. TAHAH clients have full access to the range of clinical and social supports offered at VNHS.
VNHS values a collaborative model of providing care, treatment and prevention and has long-term, established partnerships with other Vancouver-based clinical and community services, such as St. Paul’s Hospital and BC Housing. TAHAH clients are given assistance to access these other services.
Relationship with the Positive Outlook Program
TAHAH is a sub-program of the Positive Outlook Program, which is also based at VNHS. The Positive Outlook Program provides care, treatment and support services to people living with HIV. In addition to nursing care and outreach services, the program offers drug and alcohol counselling, social work services, maximally assisted medication therapy, daily breakfast and lunches, a weekly food bank and a rent supplement program. It is open seven days a week, so TAHAH clients can access the Positive Outlook Program on the weekends, when TAHAH is closed.
Many TAHAH clients access some form of services from the Positive Outlook Program, such as its breakfast and lunch program or its drop-in space. TAHAH staff are able to check in with and monitor their own clients when they visit the Positive Outlook Program. The two programs also case conference together every morning; this unique relationship is very important as is allows for continuity of care for clients and support for staff.
Peer health advocates
Peer health advocates are a critical component of TAHAH. The program employs four peers, each of whom work four hours per week. All of the TAHAH peers are clients of the Positive Outlook Program and were initially engaged in peer work via a 2005 community-based research project partnership with Simon Fraser University. This partnership offered peers a year-long community-based researcher training program, which gave the peers a foundation of knowledge and skills related to the peer role.
Most of the peer health advocates, who themselves still experience many of the challenges faced by TAHAH clients, have been working with VNHS since 2006. This is a significant demonstration of their commitment to their work.
The case manager or a nurse checks in with the peer health advocates weekly to debrief, identify areas for improvement, solve problems and ensure that the peers are engaged in active self-care work and burnout prevention.
TAHAH is in the process of reinvigorating its support system for peer health advocates to help them to provide the best possible services for TAHAH clients. Given the small caseload of TAHAH, the commitment of the existing peers and the intensity of the peer training, which cannot be replicated easily, TAHAH does not recruit new peer health advocates.
Identifying potential TAHAH clients
TAHAH clients are First Nation people living with HIV in extremely marginalized circumstances and in a state of significant instability. This instability may relate to their HIV status (e.g., they may not be adhering to antiretroviral therapy or may be unable to start it), but it may not. It may also relate to other health or social aspects of their lives (e.g., issues with adherence to methadone; homelessness.) Almost all clients are living with addiction and some live with mental illness.
All TAHAH clients are referred to the program by a healthcare provider, usually the VNHS physician or a Positive Outlook Program staff person. Less frequently, the referral comes from a member of the STOP outreach team.The people who provide the referrals recognize the instability described above and refer clients who require more support than their services can provide.
Once a person is identified as possibly being interested in the services that TAHAH provides, a more intensive engagement process begins. A TAHAH nurse and the case manager will engage the person at VNHS, in their home or on the street, depending on the circumstance. For example, they may approach the referred individual while they are visiting the Positive Outlook Program to tell them about TAHAH. Other times they may visit a person out in the community while they are on outreach. In all cases, the purpose of the first contact is to introduce the program and start to build trust between the person and TAHAH.
Initial and ongoing client engagement: building trust and stability
Although one of the main goals of the TAHAH program is to reduce HIV transmission by ensuring access to HIV treatment, considerable work must often be done to help the client to build stability before they can be ready to consider HIV treatment. Stabilization can include addressing the client’s fundamental survival needs, such as housing and food, and addressing their other health issues.
Once a person is identified as a possible TAHAH client, the nurses and case manager begin a gentle but thorough assessment. By using a medicine wheel intake form, they are able to develop a comprehensive picture of the client and start to develop a care plan. However, given that most new TAHAH clients are managing multiple complex issues, it is rare that the intake process is conducted in one visit. Rather, the team works through the assessment over time, so as not to overwhelm the client.
TAHAH is very flexible and carries out different activities each day to meet the unique needs of individual clients. Each morning, the nurse on duty and the case manager at TAHAH meet first with the Positive Outlook Program staff team, as all TAHAH clients are also Positive Outlook Program clients, and then on their own, to discuss client needs and develop a plan for the day. It is during these discussions that the nurse or case manager may determine that a peer health advocate should be engaged in a client care plan. However, not all clients work with peers. The decision to involve a peer is based entirely on the unique needs of the client.
Although each person’s relationship with TAHAH is different, after intake a person is typically engaged in intensive case management where their immediate needs are met. For instance, they may be given access to safe housing, treatment for infections and wound care. Clients will also be supported to have initial (and then ongoing) viral load and CD4 tests to assess their health in relation to their HIV infection. TAHAH staff will liaise with family physicians, specialists, peer health advocates and other external health and social service providers, to ensure that clients are receiving the comprehensive care that they require. The support is intensive and very responsive to the client.
TAHAH connects with clients through a combination of approaches. Clients can drop in to access the services of the case manager, but most of the support work happens on the street and in people’s homes. The nurses, the case manager and the peer health advocates do considerable outreach work, checking in with TAHAH clients and attending to pressing health crises. During both clients’ drop-in visits to TAHAH and TAHAH staff members’ outreach interactions, the clients are often concerned about issues that are more acute and immediate than their HIV status, and these frontline interventions also help to build a solid relationship. Genuine and therapeutic connections flourish in this context; these connections, in concert with increased access to survival supports, such as food and shelter, nurture TAHAH clients in their progress toward improved well-being.
On-site HIV treatment and access to healing
TAHAH clients have access to HIV specialists, family physicians, nurses and a variety of allied healthcare professionals on site. First Nation traditional knowledge, supports and ceremonies are also available in the clinic, often via an elder, which can really make a difference in a client’s ability to access Western health and social services. The TAHAH team will work with a client for months through intensive care management, clinical care and system navigation to build stability in their life and help them to become ready for antiretroviral therapy. This work includes providing ongoing education about the challenges the client may face while on treatment, particularly during the first month of treatment. For clients who are particularly hesitant to start treatment, peer health advocates can be very helpful at this stage of care, as they can talk, peer to peer, about what it is really like to start HIV treatment.
When a client chooses to access HIV treatment, they will work closely with the on-site HIV specialist and undergo appropriate resistance and genotype testing before starting a regimen. Clients typically access medication in one of two ways: through a pharmacy located next door to VNHS, with which VNHS has a very good relationship, or through the Positive Outlook Program’s medication program. For those who do not show up to pick up their medication at the Positive Outlook Program, staff will conduct outreach to try to deliver it to them. If staff members are aware that a client has run out of medication and they cannot locate them to give them more, they will notify the client’s physician.
By providing intensive case management and ongoing clinical monitoring, along with access to First Nation traditional care, TAHAH staff members help clients to adhere to their treatment regimen and can determine if a client’s care will need to be changed (e.g., changing the treatment regimen or the intensity of support). The on-site physicians and infectious disease specialist work closely with the team and the client to monitor treatment uptake and progress.
The activities outlined above are part of an intensive one-on-one model of care that focuses on client-centred care and client autonomy. While TAHAH aims to support clients with education, support and peer counselling, it also promotes the value that clients have the right to choose and to make informed decisions about their health and well-being.
“Graduation” from TAHAH
Once a client has remained stable in multiple aspects of their lives (e.g., they have been stably housed and on HIV treatment for a period of time), they are able to graduate out of the program. Typically, people only graduate from TAHAH when they are stable and/or move out of the Downtown Eastside community (and cease to access services at VNHS.)
It can take a long time for clients with complex life realities to build a secure and stable foundation for their lives. The TAHAH team must work at a pace that is suitable for the client and on the issues that are most important to the client. Although some people do move on, graduation rates are low because of the length of time it can take for some people to stabilize. The TAHAH team members are committed to the relationships that they build with clients over the long term and they will continue to provide support as needed. However, the low graduation rate had been a challenge for TAHAH given that the program has capacity for only a small caseload—if none of the existing clients graduate, the program is unable to take on new clients. TAHAH typically graduates one or two people per year.
Required Resources
Human resources
TAHAH is staffed by one full-time nurse (this position is filled by two part-time employees); one intensive case manager, who works 32 hours per week; community health advocates, who each work four hours per week; and one elder, who works 10 hours per week for all VNHS programs.
TAHAH staff work closely together in a coordinated and non-hierarchal leadership model. The individuals in each position bring a particular range of expertise; however, there is considerable fluidity across the roles in terms of how connections are made with clients and supports are offered.
All TAHAH staff, first and foremost, work to build and maintain relationships and trust with clients. There are additional responsibilities associated with each position, as discussed below.
The role of the nurses is to triage the most critical health issues facing the client, which often are unrelated to their HIV status. By providing immediate and necessary health care, the nurses establish trust and engage clients in therapeutic and educational dialogue. They also encourage the client to have blood work done to help monitor the client’s HIV viral load and CD4 counts and provide them with information about treatment options. In addition, the nurses provide reminders for and will accompany clients to physician appointments.
The case manager’s role is focused on increasing the client’s access to services to support stabilization. These services often include housing, food and disability benefits. The case manager also gives reminders for and will accompany clients to doctor and specialist appointments. By providing intensive case management, they connect all the aspects of client care.
The TAHAH Elder is well known and respected in the Downtown Eastside. The elder’s involvement in the program provides an essential pathway to First Nation knowledge, traditions and ceremonies, things that are often highly valued by clients and in short supply in their lives. This assistance in reconnecting to First Nation cultural traditions can be a source of strength and healing for First Nation clients. The elder also supports the peers and the rest of the TAHAH team practically and philosophically by promoting indigenous knowledge in the care and support of the program’s clients.
The peer health advocates are Positive Outlook Program clients and each identify as a First Nation person living with HIV. Two of the four health advocates still live in the Downtown Eastside. They are responsive to clients’ needs and support clients in a variety of ways. Sometimes clients are living in extreme isolation and the peer health advocates can act as surrogate family members. The peers visit clients in the hospital, talk to them about HIV treatment and living with HIV, accompany them to appointments and help them learn the ropes as they begin to access the available resources.
Challenges
- The time needed to build relationships. TAHAH clients’ experience of historical and institutional trauma is correlated with their lack of trust of health and social services. Further, many experience instability that prevents them from being able to participate in formalized services. As a result, building relationships takes considerable time— possibly more time than would be needed within other communities.
- The transient nature of the population. The realities of client transience and a local housing shortage present challenges to TAHAH service delivery. Clients need stable housing if they are to make regular connections.
- Challenges associated with maintaining the therapeutic relationship. It is as challenging to maintain a therapeutic relationship with a TAHAH client as it is to establish it. Staff must stay patient, intentional and assertive while working at the pace set by the client and respecting their priorities. Over time, the client’s and the community workers’ priorities align toward a commitment to accessing services; this alignment evolves naturally as clients feel respected by their workers and as their basic needs for things like housing, food and community are increasingly addressed.
- Human resource issues. Hiring and retaining qualified and capable staff is an ongoing challenge. TAHAH’s clients manage multiple issues, and supporting them requires significant human resource hours. As a result, TAHAH maintains a small caseload and restricts its participant intake process to those who are in most need of services.
- Ethics of patient autonomy. There is often debate about the ability of patients to make the “right” decisions about their well-being when they have untreated mental illnesses, developmental challenges, acute addictions or combinations thereof. This is an ongoing challenge for staff members trying to understand decisions about refusing treatment and care, especially by clients who are ill and/or dying. In the future, it would be helpful for TAHAH to engage a part-time consultant, on an as-needed basis, who specializes in ethics, cognitive impairments, mental health and/or patient autonomy.
- Challenges for peer health advocates. It has been a challenge for all of the peers on staff to transition from solely being participants at the Positive Outlook Program to being valued, peer support workers. For the rest of the TAHAH team, there was a learning curve regarding the amount of supervision and support required (or not required) by the peers and how to recognize former “clients” as employees who now had access to office space and files that previously had been off limits to them. The peer health advocates needed to get accustomed to the responsibilities of their new positions, including self-care and support for one another in their work. Hiring peers as community health advocates requires significant resources in terms of staff support, training and supervision.
- Challenges associated with incorporating First Nation culture(s) and healing practices. The inclusion of First Nation culture(s) and healing practices is critical, but not always easy. Although TAHAH is situated on traditional Coast Salish territory, defining what constitutes “Aboriginal” healing practices is a challenge when working with very diverse, urban First Nation peoples, many of whom do not share cultures, histories or languages. Furthermore, “pan-Indian” stereotypes are often applied to all First Nation communities; TAHAH works to deconstruct these beliefs. It is also a challenge for Western practitioners to create and ensure the professional space required for First Nation cultural knowledge and practices.
Evaluation
TAHAH is required to conduct ongoing evaluations of clinical indicators of client well-being as part of its funding arrangement with the Vancouver STOP project. TAHAH staff also report on the following:
- the number of clients actively receiving support from TAHAH
- the number of clients who graduate from TAHAH
- the number of clients engaged in care with a family physician (at VNHS or elsewhere)
- the number of clients who are on HIV treatment with a viral load of less than 200 copies/mL
- the number of clients with CD4 counts less than 200 cells/mm3 who are not on antiretroviral therapy
- the number of clients who have completed social housing and/or disability benefit applications
- the number of clients placed in social housing and/or on disability benefits
- the number of clients who claim to be food secure.
TAHAH assesses its success using both the indicators outlined above and staff’s perception of how well their clients are moving toward long-term stabilization, which is a challenging thing to gauge. They evaluate this progress by looking at and celebrating both small and large positive changes in individual people’s lives, such as indications that a client’s priorities are increasingly aligning with a commitment to accessing healthcare and related services.
Lessons Learned
- Knowledge of First Nation histories, cultures and philosophies of health is critical. Health providers must be supported to develop awareness of the historical context and cultures of First Nation peoples in Canada and their perception of heath. Health is understood by First Nation people as more than just absence of illness, and their understanding of health is also affected by historical and personal experiences of colonization.
- It takes a lot of time to build and maintain therapeutic relationships, but it’s worth it. Building therapeutic relationships with people who distrust health systems and have experienced trauma can take time, but these relationships are essential in supporting clients to experience a broader range of health choices.
- Peer health advocates can connect with clients in a different way. Peers offer education while modelling the skills necessary to navigate the extremely complex texture of street life, HIV infection and substance use.
- Programs must be flexible to respond to client needs. TAHAH continually evolves to adapt to its clients’ needs and views health as a lifelong process that unfolds in incremental stages. Healing in relation to HIV infection, trauma, substance use and addictions is understood as a process. A metaphor that is often used is that TAHAH staff members “walk beside” clients on their healing journeys.
- Multidisciplinary healthcare teams are required to provide the best care. On-site specialists facilitate a comprehensive approach to health issues and low-barrier referral processes.
- The social determinants of health must be addressed. Without safe and affordable housing, a reliable source of income, and a family doctor who understands the complexities of addictions, mental illnesses and poverty-related illness, it is impossible for a person to participate in their own healthcare decisions, such as starting HIV treatment.
Program Materials
Contact Information
TAHAH
Case manager: 604-369-5996
Nurse: 604-369-3640
Positive Outlook Program 604-254-9937
Vancouver Native Health Society
441 Hastings Street East
Vancouver, BC, Canada
What is the STOP HIV AIDS Project?
Seek and Treat for Optimal Prevention of HIV/AIDS (STOP) is a $48 million, four-year pilot project funded by the government of British Columbia. This project aims to increase the quality of life of people living with HIV and to reduce the number of new HIV infections by taking a proactive public health approach to finding people living with HIV, linking them to HIV care and treatment programs and supporting them to stay in care. STOP aims to improve the experience of people living with HIV or AIDS in every health and social service interaction, and significantly improve linkage and engagement across the full continuum of HIV prevention, testing & diagnosis, treatment, care and support.
STOP was rolled out in Vancouver and Prince George. It was made up of numerous interconnected and discrete clinic-based, hospital-based, community-based and policy-focused programs implemented through the collaboration of a significant number of stakeholders. In Vancouver, Vancouver Coastal Health and Providence Health Care partnered to form the Vancouver Project. Through this partnership, these two organizations shared governance, funding and reporting for many of the initiatives that took place in Vancouver between 2011 and 2013.
In 2011, the TAHAH project received Vancouver STOP Project funds to support the program, which up to that time had existed only as a research project. These resources allowed TAHAH to continue beyond the timeline of the research project by providing ongoing funding for the research project’s case manager, peer health advocate and elder positions. Nursing positions had been a part of the TAHAH research project in earlier years, but more recently the project had not been able to fund this role. The STOP funds enabled TAHAH to strengthen its ability to serve its clients by hiring two Vancouver Coastal Health nurses to work at TAHAH part time. These part-time nursing positions have had an added benefit: with Vancouver Coastal Health nurses now embedded in TAHAH, Vancouver Coastal Health has been able to develop a unique relationship with the program.