What is the program?
The Calgary Drop-in Centre, a large inner-city shelter, provides low-barrier, integrated hepatitis C care for people who use drugs through the hepatitis C program. This program is a partnership between the Calgary Drop-In Centre, CUPS Calgary Liver Clinic and Mint Health + Drugs Pharmacy, a community pharmacy.
The Calgary Drop-In Centre is a large, low-barrier shelter that has in-house healthcare services. In addition to offering housing services to their homeless clients, they also provide care for complex medical needs, including addiction, mental health and chronic health conditions. The centre’s staff work directly with a pharmacist from Mint Health + Drugs. The CUPS Liver Clinic provides low-barrier hepatitis C care through a harm reduction approach, as well as other education, prevention and care for people with chronic liver disease (e.g., cirrhosis, alcoholic fatty liver disease).
The hepatitis C program provides hepatitis C testing and treatment services entirely within the walls of the Calgary Drop-in Centre. Integrating hepatitis C care into this shelter has created better access for marginalized individuals, including people experiencing homelessness and people who use drugs.

Why was the program developed?
The Calgary Drop-In Centre provides services to people at high risk for hepatitis C, including:
- people who use drugs
- people experiencing homelessness
- people with a history of incarceration
- people with current/past mental health issues
- people who have barriers to accessing mainstream health care
Before the hepatitis C program was introduced, the centre’s clients were having difficulty connecting to hepatitis C testing and treatment in the community. Barriers related to substance use, housing, transportation and health literacy led to missed appointments. In addition, people who use drugs may avoid seeking care from providers and settings that they are not familiar with because they often face stigma in the healthcare system. Although the CUPS Liver Clinic is located near the Calgary Drop-In Centre and uses a harm reduction approach, many of the shelter’s clients were not making it to the clinic.
On the basis of these observations, a partnership was developed between the Calgary Drop-in Centre Health Services team, an outreach pharmacist from a community pharmacy and the CUPS Liver Clinic. They developed a model of integrated care where shelter staff were trained to test clients for hepatitis C and connect them to care and treatment within the shelter.
This program was framed as a “micro-elimination” project: the Calgary Drop-in Centre was targeted as a setting to ramp up hepatitis C testing and treatment with remote support from the CUPS Liver Clinic team. Additional funding was provided from public and industry grants to cover the hepatitis C training and a portion of the staff’s hours.
How does the program work?
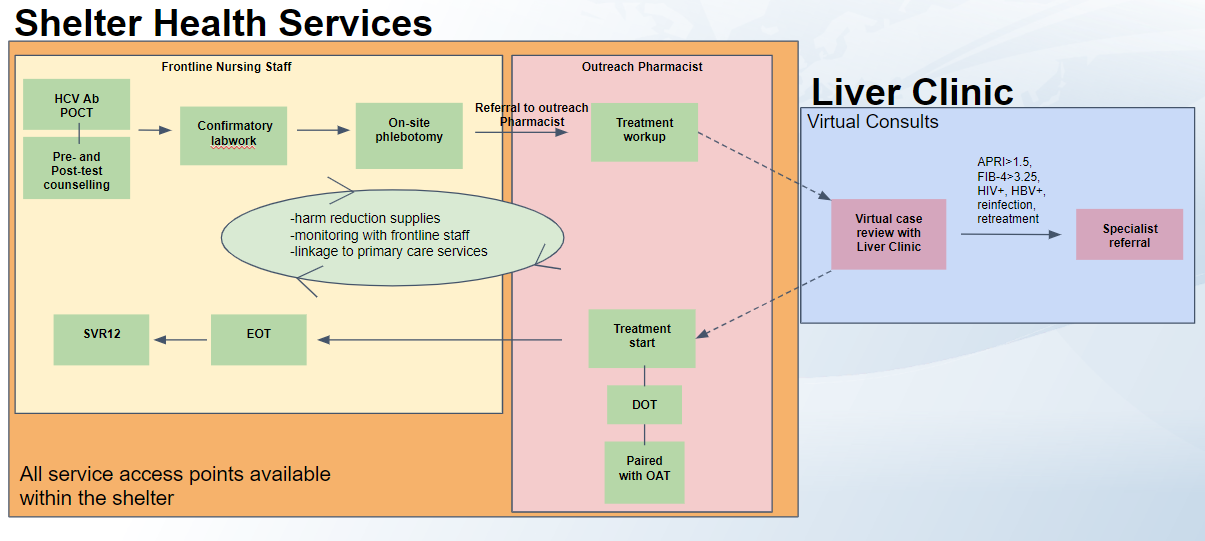
The hepatitis C program at the Calgary Drop-in Centre launched in early 2021 in partnership with the outreach pharmacist and CUPS Liver Clinic staff. In the program, a multidisciplinary team provides hepatitis C testing and treatment services entirely within the walls of the shelter. Shelter staff were trained to deliver hepatitis C testing and treatment, with remote clinical support provided by staff from the CUPS Liver Clinic. The program developed a clear process that outlines specific phases of treatment, as well as who is responsible for each phase. More clinically complex cases are referred to the CUPS Liver Clinic for further assessment and treatment planning (e.g., individuals with HIV, hepatitis B or extensive liver injury). Treatment planning can happen remotely and if a client is referred to the CUPS Liver Clinic for an in-person visit they can receive support (e.g., bus tickets, follow up reminders from Shelter staff) to assist them in attending their appointment.
Training shelter staff in delivering hepatitis C services
Before the program launch, the CUPS Liver Clinic nurse and outreach pharmacist held a series of in-person trainings with Calgary Drop-in Centre staff, including nurses. This training was for any healthcare staff who would be delivering hepatitis C services, including testing. The training focused on:
- mechanisms of hepatitis C infection and disease progression
- updates on hepatitis C treatment and direct-acting antiviral therapy
- context of hepatitis C elimination
- point-of-care (POC) testing, including pre- and post-test counselling
- connecting clients to other primary care services
- harm reduction and trauma-informed practice
Testing and linkage to care by nurses
Frontline nursing staff at the shelter are the first people at the shelter with whom clients have contact, and clients often already have trusted or familiar relationships with them. In collaboration with the outreach pharmacist, the nurses provide point-of-care testing for individuals at risk of hepatitis C, including those with past or ongoing substance use. If the point-of-care test result is positive, additional blood draws are done for a confirmatory RNA test. Point-of-care testing and blood draws take place in the shelter’s health clinic, and RNA test samples are sent to a central laboratory. The nurses are trained in phlebotomy and are able to complete all required blood work on site. Testing also provides an opportunity to educate clients about hepatitis C even if their test result is negative.
Those who receive a positive test, as well as individuals who had a previous, untreated hepatitis C diagnosis, are linked to treatment within the shelter.
Developing a treatment plan
The outreach pharmacist leads the treatment, patient counselling and any work-up, including paperwork for insurance coverage. In Alberta, pharmacists have the authority to prescribe certain drugs, including hepatitis C medication for non-complex cases.
The outreach pharmacist then communicates via an electronic medical record system with the CUPS Liver Clinic nurse and physician to create a treatment plan. If there are complex clinical considerations (e.g., HIV or hepatitis B coinfection, extensive liver injury), clients are referred to the CUPS Liver Clinic to be treated by hepatitis C nurse and specialist physician. Otherwise, treatment is delivered at the shelter. The pharmacist dispenses hepatitis C medication, often alongside opioid agonist therapy or other daily medication. Individuals can also receive weekly or monthly supplies of medication if they are not using shelter services day to day.
Supporting treatment and successful cure
Health services staff at the shelter monitor adherence and provide on-treatment support. Many of the clients who are on treatment visit the shelter daily, so the staff have a close working relationship with them. Individuals also receive other wraparound supports, including primary care, harm reduction supports and other services through the Calgary Drop-in Centre.
Twelve weeks following the completion of treatment, a nurse tests the individual to confirm successful cure.
Required resources
- Frontline shelter nurses
- Other shelter health services staff
- Outreach pharmacist (prescriber)
- Liver Clinic nurse
- Liver Clinic physician
- Online communication tools
- Training curriculum for shelter staff
- Other wraparound services including primary care, harm reduction and housing
Challenges
- The COVID-19 pandemic: Healthcare providers have been stretched thin by the COVID-19 pandemic, with many being reassigned to different roles. Reduced capacity meant that hepatitis C services were less of a priority, particularly for many shelter staff. Additionally, certain provincial restrictions added barriers to accessing hepatitis C care and treatment, including laboratory closures and a backlog of medical coverage requests.
- Losing people to follow-up: This program works with highly marginalized populations that face issues related to homelessness, substance use or mental health. Although this program is a low-barrier, integrated model, individuals may be lost to follow-up. The program mitigates this risk by staying flexible, maintaining close contact with other service providers an individual may be working with, and revisiting hepatitis C treatment options if a client re-engages with health services.
- Ongoing barriers to hepatitis C treatment: Outside of this program, there continue to be ongoing barriers to accessing hepatitis C treatment in Alberta. These include long wait times for blood work results, requirements for recent RNA results within 6–12 months of applying for treatment and other issues related to treatment coverage. There also continues to be both client and provider stigma about hepatitis C and a general lack of hepatitis C treatment providers. Similar programs to this one that can be led by other prescribers in community settings may help to address this.
Evaluation
From the launch of the program in March 2021 to October 2021:
- 61 patients were tested using hepatitis C point-of-care testing*
- 11 patients completed or were undergoing treatment
- 3 patients were in the process of treatment work-up
- 19 shelter health care workers completed hepatitis C training
*Note: Point-of-care testing is used to find and diagnose new cases, and it is also used as an educational/outreach tool. Many people who initiated treatment in the program had had previous diagnoses and were not necessarily identified through this program.
Lessons learned
- Removing siloes in hepatitis C care: Decentralizing care from a specialty clinic opens up the possibility for marginalized people to be cured of hepatitis C. By collaborating across agencies and physical locations, this program was able to remove physical barriers to hepatitis C testing and treatment that allowed individuals to access care in their “health home.”
- Communication is key: Consistent and clear communication between program partners was crucial to this program. Although there was little in-person contact between the two sites, shelter staff had the ability to remotely access the CUPS Liver Clinic electronic medical record system and use it to effectively communicate about program and patient information.
- Having a clear plan with defined roles: Investing time at the beginning of the process to create a clear treatment workflow, along with assigned roles and responsibilities, was crucial for clarity and cohesion. Having a clear process in place reduced delays and confusion and created more streamlined care for patients. Ensuring that data collection processes were in place and completed was also key in program evaluation.
Program materials
Contact information
Kate Newcombe
Registered nurse
CUPS Liver Clinic
kate.newcombe@albertahealthservices.ca
Nicola Gale
Clinical pharmacist
Mint Health + Drugs
nicola.g@mintdrugs.com
