- Safer injection 101
- Safer injection supplies
- Choosing an injection site
- Tips for safer injection
- After injecting
- Potential harms and how to recognize them
- The importance of scoring and injecting for yourself
- Keeping safe during the overdose crisis
- Stimulant overamping
- Stimulant overdose
- Opioid overdose
- Responding to a suspected overdose
Safer injection 101
The following tips are based on the proven best practices for safer injection. You can use these tips in your day-to-day life to keep healthy and stay safe. Not all of these steps can be followed all the time by everyone, but staying as close to safer practices as possible lowers the chance of health issues.
Everything new every time you use.
- Use new needles, syringes, filters, water and cookers every time you inject drugs.
- Use your own gear, don’t share with others, and follow steps for safer injecting to lower your chance of damaging your veins and getting bacterial infections or viruses that are passed through the blood, like hepatitis B, hepatitis C and HIV.
Reduce the chance of a fatal overdose.
- The best way to prevent a fatal overdose is to not use alone. Have at least one person you trust with you, ask someone to check in on you when you’re using, or use at a safe consumption or overdose prevention site.
- Stagger use with other people so someone is able to respond if an overdose happens.
- Carry naloxone, know how to use it and let others know you have it. Keep your naloxone in a place that is easy for others to find in an emergency.
- Start low, go slow. Use a small test dose first. It may take a few moments for the drugs to take effect, and they may be stronger than you realize.
- Know the source of your drugs and inject yourself. Take control of your own use by knowing the source of your drugs and learning to inject yourself safely. Some harm reduction organizations offer drug testing.
Take a break and take care of yourself.
- Be kind to yourself, your skin and veins.
- Take breaks and get some sleep.
- Eat something before you use. Stay hydrated with water or juice.
- Have condoms and lube with you.
- Take care of your veins and use different sites.
Safer injection supplies
Using pre-packaged, single-use supplies will help to prevent bacterial infections and lower the chance of passing viruses such as hepatitis B, hepatitis C and HIV. Harm reduction organizations may be able to supply these safer injection supplies, as well as provide support and other information.
- NEEDLES AND SYRINGES - Needles and syringes come in different gauges, sizes and lengths.
- ALCOHOL SWABS - Alcohol swabs are used to clean the skin before injection.
- COOKERS - Cookers are used to prepare drugs for injection. The drugs are mixed with sterile water (and in some cases, vitamin C powder) in the cooker. This mixture may be heated to help dissolve the drugs into a liquid and to prevent infection from certain bacteria.
- STERILE WATER - Sterile water is used to dissolve drugs for injection. It comes in single-use packets.
- ACIDIFIERS - Vitamin C powders, ascorbic acids or “acidifiers” are only necessary for drugs that won’t dissolve in sterile water alone. Some examples are brown/black tar heroin, crack cocaine and fentanyl patches.
- FILTERS - Filters are used when pulling drugs into a syringe from the cooker. Using a filter prevents undissolved solid particles from getting into the syringe and into your body, especially when you are injecting a crushed pill with a coating.
- TIES OR TOURNIQUETS - Ties and tourniquets (sounds like “turn-a-key”) restrict blood flow, making the veins bulge out and easier to find.
- DRY SWABS - Dry swabs, bandages or Band-aids are used to cover and put pressure on the site after you’ve injected.

Choosing an injection site
There are some places on the body that are safer to inject into than others. Injecting can cause serious harms, such as vein damage, a blood clot or too much bleeding that won’t stop.
Safer:
- Arms: Your arms are the safest places to inject (above the wrists to below the shoulder). Rotating your injection sites and the veins you use will help them heal faster and prevent infection.
- Back of hand: The veins in this area are fragile. To keep them healthy, inject slowly, remove the tie or tourniquet before injecting and give these veins extra time to heal.
Proceed with caution:
- Legs: Injecting in your legs has a higher risk of blood clots. There will be serious problems if a clot travels into your lungs or heart. Injecting in spots lower on your leg (below the knee) is a way to reduce this risk.
- Feet: The veins in this area are very fragile. To keep them healthy, give these veins extra time to heal and choose other sites if you have foot problems.
- Breasts: Injecting into your breasts can cause blood clots that cause pain and swelling. There will be serious problems if a clot travels into your lungs or heart.
Dangerous:
- Neck: The veins in your neck are very close to large arteries that send blood to your brain. Injecting into your arteries can cause life-threatening complications like blood clots, bleeding and rapid swelling.
- Wrist: Your wrists are full of veins, arteries and nerves that are very close together. Injecting into an artery or nerve is painful and can cause serious health problems.
- Groin: The veins in the groin are very close to large arteries that provide blood to your legs. Hitting these arteries is more likely to result in major bleeding, which is very dangerous. If you do inject here and get a big bruise, get medical help right away.
- Genitals: The veins in your genitals are delicate and difficult to see. Since the blood vessels in this area are so small, they are easily damaged if you try to inject into them and they are prone to infection.
Remember: Use veins to inject. It is dangerous to inject into an artery. To make its way around your body, the blood in your arteries is pumped at a very high pressure – some of your larger arteries have a pulse that you can feel with your fingers. You’ll know if you’ve injected into an artery because it will really hurt. The pressure in the artery will force the plunger backwards and the blood inside your syringe will look foamy. If this happens, take the needle out right away and press down hard on the site until the bleeding stops. If the bleeding doesn’t stop in five minutes, you need to go to the hospital right away.
Tips for safer injection
Injecting drugs can result in harms to your body, including damage to your veins and bacterial and viral infections. Following safer injection practices can reduce these harms.
Preparing your drugs
- Wash your hands with soap and water before you open any of your supplies. You can also use alcohol swabs, but make sure you always have a few available for when you inject.
- Prepare your drugs in a place that is clean and has good lighting. Take your time to clean your preparation surface and do not rush when injecting.
- Find the right needle size for you. It may take some trial and error, but it is important that you find a needle size (or gauge) that works best for you. It’s recommended that you start with a small needle size first. This will help reduce track marks, swelling and bruising. If you find that you end up poking yourself many times before you’re able to inject, you could be damaging the vein. If this is the case, try using a slightly larger needle size.
- Use sterile water to mix your drugs. Sterile water in packaging that has been broken or has holes is no longer sterile and should be thrown away.
- If you are using vitamin C powder to dissolve drugs like crack cocaine or tar heroin for injection, start with a very small amount. Use the smallest amount of vitamin C powder possible to prevent the mixture from getting too acidic, which can damage your veins and cause infection.
- Cooking your drugs can help to dissolve drugs for injection and can kill certain bacteria. The drugs are mixed with sterile water (and in some cases, vitamin C powder) and often heated in the cooker. It’s important to heat the mixture for at least 10 seconds and let your drugs cool down before you inject, as hot drugs can burn your skin and damage your veins.
- Filtering your drugs helps remove any fillers or particles that did not dissolve when drugs were cooked and may cause harm when injected.
- Keep your equipment sterile while using. Supplies come in sterile, single-use packages. Don’t put your needle and syringe down once you’ve opened (uncapped) them. This will help lower the chances that your equipment comes in contact with dust, dirt or bacteria.
Preparing your injection site
- Tie a tourniquet above the place where you’ll inject – at least five inches away from your injection site. Be sure to remove it before you start to inject.
- See or feel the vein before you try to inject. It is important to inject directly into the vein. This will help prevent abscesses, scarring and infection. Keep in mind that some drugs, like crack/cocaine, have a numbing effect, which makes it easier to miss shooting into a vein if the injection site has become numb from a previous injection.
- Clean your injection site with an alcohol swab before you inject. These swabs are for a single use only, so it is helpful to have a few on you in case you need to switch to a different site or want to prepare a few sites in advance. Let the area air dry before you inject, so that you don’t irritate your skin or veins.
Ways to find a vein
It’s important to inject directly into the vein to prevent harms. Here are some ways to make your veins bigger and more visible:
- Drink water or juice before injecting.
- Clench and relax your fist and gently slap the skin.
- Apply a damp, warm cloth over the vein.
- Your local harm reduction organization may have a vein finder that you can use. This uses a special light to locate your veins.
- Tie a tourniquet above the place where you’ll inject – the further away, the better. Be sure to remove it before you start to inject.
Injecting
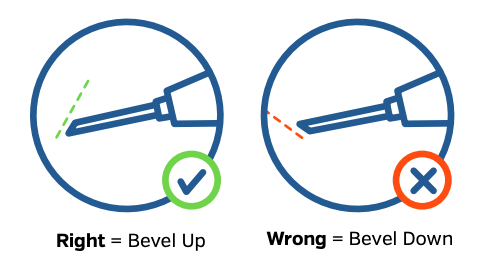
- Bevel up! The bevel is the sliced angle at the end of the needle. It’s easier and safer to inject with the bevel facing up (the sharpest point of the needle pointing down).
- Go with the flow, towards your heart. When injecting, insert the needle in the same direction that the blood flows in your veins – towards the heart.
- Flag to make sure you’re in the vein. Pull back on the plunger until you see blood in the syringe – this means you’re in the vein. If no blood can be seen in the barrel of the syringe, remove the needle and try again.
- Once blood appears in the syringe, untie the tourniquet before you inject. You can do this by pulling the tucked end.
- Start low, go slow. Use a small test dose first and inject slowly. It may take a few moments for the drugs to take effect and they may be stronger than you realize.
After injecting
- Remove the needle and apply pressure to the site after you’ve injected, using a sterile dry swab or compress. Leaving the needle in the vein is dangerous, because you can nod off and cause damage to your vein.
- Dispose of used equipment in a community drop box or personal sharps container. This will help prevent any accidental needle stick injuries to yourself and others in your community.
After injecting
Vein care
Caring for your injection sites makes a world of difference for your veins and overall health.
- Giving your veins a holiday every once in a while and rotating places where you inject will give your veins time to heal and lower the chance of scarring and vein collapse.
- Using a vein cream on your skin helps to reduce swelling and track marks. Some harm reduction organizations will have this available or give you tips on what you can use at home.
- Seeking help from a healthcare provider or harm reduction worker if you have any pain or if you get an abscess is an important way to prevent complications. Missed shots (missing the vein when you inject) and abscesses can progress to something more serious, so it’s important to seek help from a healthcare provider early.
Disposing of used equipment
Disposing of used needles and other equipment is an important step to safe injecting. This will help prevent any accidental needle sticks to yourself and others in the community.
You may have access to needle drop boxes in your community (community health centres, harm reduction organizations, public spaces like parks) where you can dispose of used equipment. Some harm reduction organizations may also be able to provide you with your own biohazard/sharps container to use at home or on the go.
Ways to plan ahead
Some people find it useful to have multiple disposal containers and to keep them in the places where they typically use. This way, the containers are there when they need them. Containers come in a wide range of sizes, so some people will carry a small container with them. This is a discreet and private way that you can safely carry used equipment until you have a chance to dispose of it properly.
Potential harms and how to recognize them
Bacterial infections
Infections can happen when bacteria enter the body through breaks in the skin. Injections cause a break in the skin.
You can reduce your risk of infection by following a few safer injecting steps:
- Cleaning your hands and site before injecting.
- Using new supplies and different sites for each injection.
- Using harm reduction filters to prepare drugs.
- Covering the site with a dry swab after injecting.
- Injecting different substances separately (such as stimulants and depressants).
If you experience signs or symptoms of infection (such as redness, warmth, increased pain), it’s important to check in with a healthcare provider or harm reduction worker.
Abscesses
An abscess is a common infection that happens as part of the body's response when bacteria get beneath the skin's surface. Abscesses are when a pus-filled bubble forms beneath the skin.
Signs:
- redness at the injection site
- swelling or raised skin
- pain and tenderness
- warm to the touch
- a giant zit with a pus-filled centre
An abscess can take a long time to heal and could turn into something more serious.
- For smaller and closed abscesses (ones that are under the skin and have not popped) or missed shots (missing the vein when you inject), apply a warm compress, keep it covered and leave it closed to prevent further infection.
- If the abscess does not improve, it could need a more direct treatment like antibiotics.
If you have an abscess, it’s important to check in with a healthcare provider or harm reduction worker.
Cellulitis
Commonly seen with abscesses, cellulitis is when the skin or the layer under the skin is inflamed because of a spreading infection. Cellulitis is often caused by missing your shot or digging around for a vein with a needle.
Signs:
- redness of the skin – the red area may get larger quickly
- warm to the touch
- tenderness
Cellulitis does not go away on its own. Applying ice or something cold to the area can help with your symptoms. Cellulitis usually requires treatment with antibiotics, so it’s important to go see a healthcare provider or harm reduction worker if you recognize the signs.
Cotton fever
The exact cause of cotton fever is unknown and it looks a lot like a blood or heart infection. The main difference is that cotton fever usually gets better on its own within 12 to 24 hours of injection.
Signs:
- fever or feeling extremely cold no matter how well you cover yourself
- feeling nauseous or sick to your stomach
- vomiting and/or diarrhea
- shakes and shivers
- terrible headache
- sweating
- twitching that feels like withdrawal or being dope sick
- fast heart rate
There is no treatment for cotton fever, and the time it takes to recover varies from person to person. Covering yourself with blankets or taking a hot shower or bath (make sure someone stays with you so you don’t drown) will help keep you warm. Medications such as acetaminophen (Tylenol) can also be used for any fever, pain or vomiting.
Heart infection (endocarditis)
When your veins are regularly exposed to fillers or bacteria, build-up occurs that may eventually lead to infection and inflammation of the inner lining of the heart.
Signs:
- chest pain or discomfort
- shortness of breath
- persistent cough
- fever
- heart palpitations (fluttering in your chest)
- fainting or weakness
- swelling of the legs or abdomen
A heart infection is very serious and could be fatal if left untreated. Treatment will most likely require antibiotics, or even surgery. If you experience these symptoms, call 911.
Skin reaction or swelling
Sometimes, people will have a skin reaction right after they inject. This typically does not last long and remains close to the injection site.
Signs:
- redness, swelling and/or bumps that form right after injection (might look like hives or blisters) that may lead to scarring
If this happens, applying ice or something cold to the area can help. Some people keep a clean wet cloth in the freezer. If the skin starts to swell or bubble, put the frozen cloth in water (to make it soft) and place it on the area. If the swelling doesn’t go down in one hour, see a healthcare provider or harm reduction worker.
Thrombophlebitis
Thrombophlebitis is when your veins are inflamed. When there’s damage to the veins, inflammation can cause a blood clot to form and block the damaged vein. This typically happens in the arms and legs. You can prevent thrombophlebitis by using the tips for safer injection, releasing the tie/tourniquet when you experience discomfort or numbness, and applying pressure to the site after injecting.
Signs:
- pain, swelling and tenderness (worse when your affected arm or leg is lowered)
- redness or swelling that follows the path of the vein
- skin that is itchy and warm to the touch
- fever
Thrombophlebitis may heal on its own but if your symptoms don’t get better or you develop a fever, you should ask a healthcare provider or harm reduction worker for help. In the short term, using an anti-inflammatory medication, like ibuprofen, as well as compression stockings will help with pain and swelling.
Viral infections
Hepatitis B
Hepatitis B is a virus that affects the liver. In Canada, most hepatitis B infections are passed through sex or through sharing of drug use equipment. This includes all injection, smoking and snorting equipment. There are effective vaccines to prevent hepatitis B.
You can have hepatitis B and not know it – most people with hepatitis B will not have symptoms in the early stages of infection. Some people will clear the virus on their own in six months, while others may develop a chronic infection, which is serious if left untreated.
Blood tests can help to identify a current or past infection. If you have not been vaccinated and think you may have been exposed to hepatitis B, you can get a test. There is no cure, but treatment for chronic hepatitis B can control the virus and decrease the chance of liver damage and liver cancer.
Hepatitis C
Hepatitis C is a virus that causes liver damage and disease over time. In Canada, most new hepatitis C infections are passed through sharing drug use equipment. This includes all injection, smoking and snorting equipment.
You can have hepatitis C and not know it – most people who have hepatitis C do not show symptoms for many years.
The only way to know if you have hepatitis C is to take a blood test. If you have shared drug use equipment with someone, it’s important to get tested for hepatitis C. Talk to a healthcare provider or harm reduction worker about where you can get tested. Treatment cures over 95% of people with hepatitis C and is much easier to take than it used to be.
There is no vaccine to protect against hepatitis C. Although there is a cure, you can get hepatitis C again. This is why it is important to use new equipment with each injection.
HIV
HIV stands for human immunodeficiency virus. HIV is a virus that can weaken your immune system, the body’s built-in defence against disease and illness. There is no vaccine to prevent HIV but there are things you can do to prevent passing or getting HIV.
The two main ways that HIV can be passed are through sex and by sharing needles or other equipment to inject drugs (or steroids or hormones).
When highly effective HIV prevention strategies are used correctly and consistently, the chance of passing HIV ranges from zero to very low. Highly effective strategies include using new equipment for injecting drugs every time, using condoms, taking pre-exposure prophylaxis (PrEP), taking post-exposure prophylaxis (PEP) and taking HIV treatment to maintain an undetectable viral load.
The only way to know if you have HIV is to take a blood test. Knowing your HIV status is very important for your health. With proper treatment and care, people with HIV can live long and healthy lives and prevent passing HIV to others. In fact, a person living with HIV who is on successful treatment cannot pass HIV to their sex partners and will lower the chance of passing HIV when injecting drugs.
Blood clots and embolisms
A blood clot forms in your veins when little particles or bacteria get into your body from an injection or part of an infection breaks off into your blood stream. If a blood clot gets loose, this is called an embolism. An embolism can travel to different parts of your body and cause serious complications.
Signs:
- If you have a blood clot in your arm or leg, you may feel pain and have redness and swelling in the area.
- If the blood clot is in your lungs, it can cause chest pain, rapid shortness of breath or loss of consciousness.
- If the blood clot is in your brain, it can cause a stroke. If this happens, you may experience numbness or weakness in a part of your body, fainting, blurred vision, problems speaking or loss of consciousness.
Blood clots and embolisms are dangerous, because they can get stuck in the vein and block the flow of blood and oxygen to important organs like your heart or brain. If you think you have a blood clot, go to a hospital right away.
The importance of scoring and injection for yourself
Not everyone is comfortable or knows how to buy their own drugs or inject for themselves and some people rely on a friend or partner to help them.
When one person has control over someone else’s drug use, it can give them a lot of power. An abusive person may also use their control to take advantage of their partner physically, sexually or financially. For example, some people abuse their partners by not helping them to inject when they want or need it or by giving them too little or too much of a drug.
This is why knowing how to score and inject for yourself puts a lot of power in your hands. Making your own connections with someone who sells drugs and knowing how to inject safely will help make sure you get what you need, when you need it.
Keeping safe during the overdose crisis
We are experiencing an overdose crisis where a toxic and unpredictable drug supply is making it dangerous for people to use drugs and making it more difficult to be safe.
The best way to prevent a fatal overdose is to not use alone.
- Carry naloxone, know how to use it, and let others know you have it. Keep your naloxone in a place that is easy for others to find in the case of an emergency.
- Use with a trusted person, ask someone to check in on you while you’re using, or use at a supervised consumption or overdose prevention site if you can.
- Stagger use with other people, so someone is able to respond if an overdose happens.
- Start low, go slow. Use a small test dose first. It may take a few moments for the drugs to take effect and they may be stronger than you realize.
- Know the source of your drugs and inject yourself. Some harm reduction organizations will have drug testing available.
Naloxone
Naloxone is used to reverse opioid overdoses.
There are two types of take-home naloxone kits in Canada:
- Naloxone nasal spray is sprayed directly into the nose.
- Injectable naloxone is injected into muscles, such as the arm or thigh.
Some provinces offer take-home naloxone kits that can be picked up for free at pharmacies without a prescription. A harm reduction organization may also be able to get you a kit.
Naloxone will not reverse an overdose from drugs that aren’t opioids, such as cocaine, benzodiazepines or alcohol, but you will not always know what is in the drugs the person has taken. If you are unsure about what kind of drug is causing an overdose, give naloxone. Giving someone naloxone will not harm them.
Overamping or overdose
Overamping or overdose is what happens when your body is exposed to more drugs than it can handle. Most drugs can be split into two broad categories:
|
Stimulants (uppers) speed the body up. These include drugs like amphetamines (such as crystal meth and speed), cocaine, crack cocaine, Adderall, MDMA, caffeine and others. |
Depressants (downers) slow the body and breathing down. These include drugs like fentanyl, heroin, oxycodone, codeine, morphine, hydromorphone, benzodiazepines, alcohol and others. |
Some of these drugs can be injected and will have different effects on your body and the kind of high you get. These effects can vary from person to person and from day to day.
The drug supply is unpredictable. There is no way of knowing how strong your drugs are and what is in them – they may include substances that you didn’t mean to use. Because of this, it’s a good idea to start with a small test amount and increase slowly.
Stimulant overamping
Overamping can happen to anyone. It results from prolonged and/or overuse of a stimulant, particularly if a person has been awake for a long time and hasn’t eaten or drunk anything in a while. Overamping isn’t fatal, but it can be upsetting, uncomfortable or scary.
Signs that someone is overamping include:
- pacing back and forth
- rapid speech
- rigid/jerking limbs
- irregular heartbeat or chest pain
- skin feeling hot or sweaty
- severe headaches
- anxiety/paranoia/confusion/agitation/hallucinations (including drug-induced psychosis)
What to do if someone overamps:
- Be calm and help the person be calm. Talk low and softly.
- Be patient and try to get them to slow their body down and rest.
- If you’re in a busy spot, help them move to a more private space where there are fewer people.
- Give them water and keep them hydrated.
- Try to help them cool down.
- Don’t leave them alone. They could be at risk for an overdose.
Stimulant overdose
Stimulant overdoses may occur following a lengthy period of use and/or if someone hasn’t rested or eaten for a while. Signs that someone has overdosed while using stimulants include:
- crushing chest pain
- seizures
- unconscious or in-and-out
- no pulse or breathing
If someone is experiencing these symptoms, call 911. They need medical attention.
Stay and help. The Good Samaritan Drug Overdose Act may protect you from arrest.
Opioid overdose
Opioids slow down the body’s heart rate and breathing. An opioid overdose can happen to anyone and opioids affect one person’s body differently than another person. An overdose may happen after periods of long use or if a person’s body isn’t used to the amount in their system. It’s important to know that an opioid overdose can happen very quickly and to recognize the signs and know when to get help.
Signs that someone has overdosed while using opioids include:
- “dropping” suddenly
- not moving and can’t be woken
- slow or no breathing
- rigid or stiff body (associated with fentanyl)
- choking, gurgling sounds or snorting
- tiny or pinpoint pupils
- blue or grey/ashen lips, nails and tips of ears (if you pinch their fingernail, the nailbed may stay white)
- cold or clammy skin
Knowing the difference between someone who is “on the nod” and someone who has overdosed
Opioids slow the body down. A person using opioids may be semi-conscious (“nodding off”) and will have a breathing rate that is slowed down. This makes it difficult for someone who is unfamiliar with opioid use to tell whether a person is experiencing a desired high or whether they have overdosed.
If someone is responsive and can speak, they do not need naloxone. Stick around - it is a good idea to continue to pay attention to how they are by continuing to check in with them and monitoring their breathing.
A good rule of thumb is that if a person can’t be woken up and they aren’t responding to you, they could be experiencing an overdose and require medical attention.
Responding to a suspected overdose
To respond to an overdose, follow the SAVE ME steps
- STIMULATE
- If someone is unresponsive, they could be experiencing an overdose.
- Try to see if they’ll respond by speaking loudly, rubbing their chest or pinching. If they do not react or respond, call 911.
- AIRWAY
- Check their airway (throat) to make sure it is clear of anything that could be blocking their breathing.
- Tilt their head backwards and lift their chin to open the airway.
- VENTILATE
- Not breathing: If the person is unconscious or has stopped breathing, give breaths. Give them one breath every five seconds. This will help oxygen get into their body and their brain.
- Not breathing AND no pulse: If a person’s heart has stopped (they have no pulse), give chest compressions in addition to breaths.
- EVALUATE
- Check to see if the person is breathing and continue trying to wake them.
- MEDICATION
- Give one dose of naloxone. Giving naloxone can help reverse an overdose if someone has opioids in their system and won’t harm someone who doesn’t.
- RE-EVALUATE AND SUPPORT
- Wait three to five minutes while continuing to give breaths (about 40 breaths) and trying to see if the person will respond.
- If no change, give another dose of naloxone. Many opioid overdoses require two doses of naloxone.
Stay and help.
- The Good Samaritan Drug Overdose Act may protect you from arrest. If you seek medical help for yourself or for someone else who has overdosed, the Good Samaritan Drug Overdose Act was put in place so that neither of you will be charged for possessing or using drugs.
- Tell paramedics as much as you can about what happened.
- If someone has responded to the naloxone, the effects may wear off in 15 to 20 minutes and they may become unresponsive again.
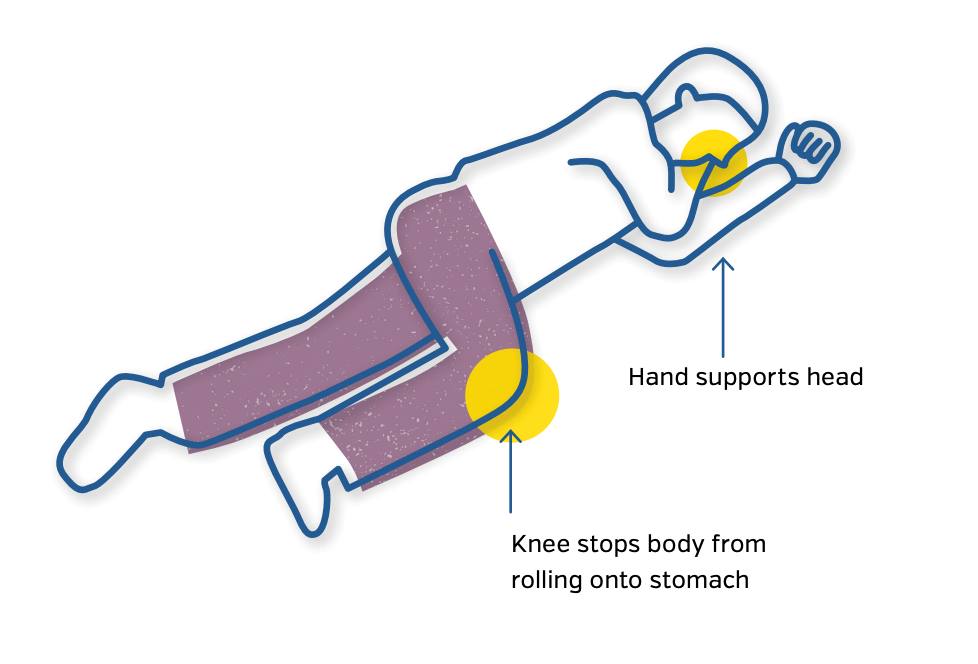
- If you have to leave the person alone, put them in the recovery position. Positioning them in this way will help keep their airway clear and stop them from choking if they vomit.
Carry naloxone, know how to use it and let others know you have it.
Thank you to Parkdale Queen West Community Health Centre, Jennifer Broad, Keith Williams and Doug Belanger from the Toronto Community Hepatitis C Program, Toward the Heart BCCDC Harm Reduction Services, Streetworks, and L'Association Québécoise pour la promotion de la santé des personnes utilisatrices de drogues (AQPSUD) for their help in the development of the resource.
Design and layout: Gravity Inc.
Copyediting: Jennifer Thomas
CATIE project lead: Shannon Elliot
This resource is adapted from a booklet by the Parkdale Queen West Community Health Centre and South Riverdale Community Health Centre, 2008.
CATIE provides information resources to help people who wish to support others or manage their own health care in partnership with their care providers. Information accessed through or published or provided by CATIE, however, is not to be considered medical advice. CATIE endeavours to provide the most up-to-date and accurate information at the time of publication.
Production of this publication has been made possible in part through financial contributions from the Ontario Ministry of Health and the Public Health Agency of Canada (PHAC).
The views expressed herein do not necessarily represent the views of our funders.

