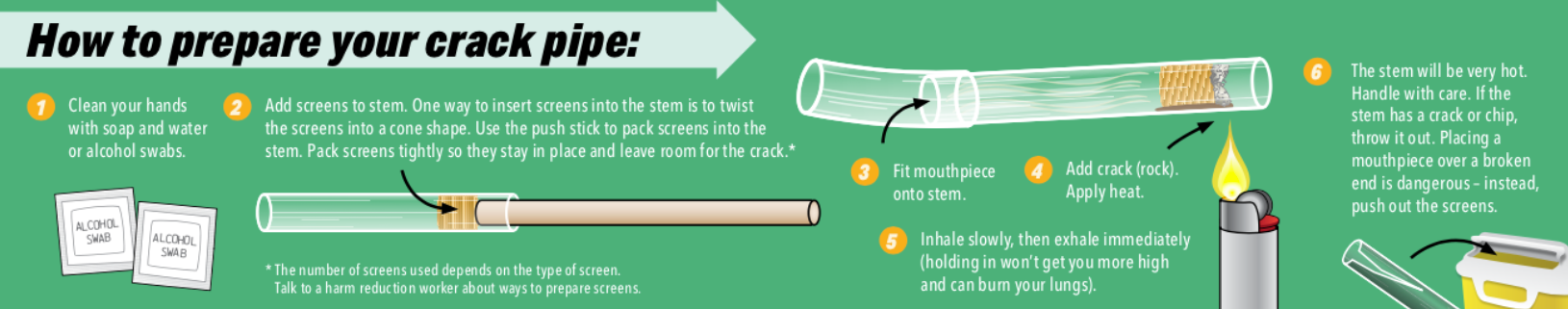
How to prepare your crack pipe
- Clean your hands with soap and water or alcohol swabs.
- Add screens to stem. One way to insert screens into the stem is to twist the screens into a cone shape. Use the push stick to pack screens into the stem. Pack screens tightly so they stay in place and leave room for the crack.
The number of screens used depends on the type of screen. Talk to a harm reduction worker about ways to prepare screens. - Fit mouthpiece onto stem.
- Add crack (rock). Apply heat.
- Inhale slowly, then exhale immediately (holding in won’t get you more high and can burn your lungs).
- The stem will be very hot. Handle with care. If the stem has a crack or chip, throw it out. Placing a mouthpiece over a broken end is dangerous – instead, push out the screens.
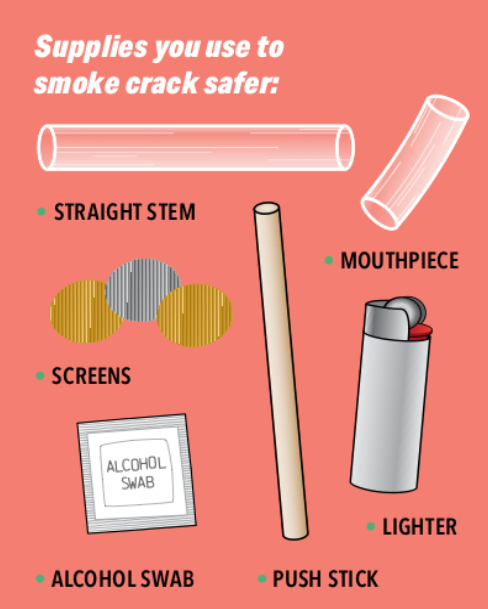
Supplies you use to smoke crack safer
- Straight stem
- Screens
- Mouthpiece
- Lighter
- Alcohol swab
- Push stick
This resource provides information about how to smoke crack with this equipment. Talk to your local harm reduction site about which safer drug use supplies are available and how they are meant to be used.
Safer crack smoking tips
- Avoid using alone.
Try to smoke in a safe place with people you trust. - Start low, go slow.
The crack may be more potent than you realize. - Check your screens.
After a couple of hits, make sure screens are still packed tightly. - Know the source of your drugs.
Try to prepare doses yourself. - Avoid mixing substances.
Alcohol while smoking crack can increase risk of alcohol poisoning. Mixing with opioids can lead to a fatal overdose. - Have condoms and lube with you.
You may want to have sex while high. - Connect with others.
Ask them to reach out to make sure you’re okay. - Take care of yourself.
Try to eat something before you smoke. Stay hydrated with water or juice. - Be kind to yourself and your skin.
Wash your hands after smoking. - Take a break.
Get some sleep, drink water or juice and eat something.
Screens vs steel wool (Brillo)
- Brass screens are much safer than steel wool.
- Small pieces of hot steel wool, such as Brillo, can break off and burn your lips, mouth and throat, damage your lungs, and can cause stomach issues.
- If using steel wool, use screens too. Put at least one screen between the steel wool and the end where you inhale. Pack the screen tightly.
- Choose the straight steel or brass kinds of steel wool, not the ones with coating or cleaning solution on them and change steel wool frequently.
Mouth care
- Drink water or juice to keep your mouth moist and reduce cracks and blisters.
- Moisten your lips with your own lip balm.
- Chew gum to keep your mouth moist and reduce clenching.
- Brush your teeth when possible or use mouthwash.
- Avoid infection by using your own mouthpiece or stem and not sharing it.
Use your own stem and mouthpiece to prevent hepatitis C
Hepatitis C can be passed through tiny amounts of blood on crack smoking equipment. Talk to a harm reduction worker about where to get equipment and where to get tested for hepatitis C. Smoking crack can lead to skin issues such as infections, lesions or abscesses that may require medical attention.
Stimulant overamping and overdose
Fatal overdoses are not common with stimulant use, however the drug supply is unpredictable and a fatal overdose is possible. Overamping can be considered a type of non-fatal overdose. This information is to help identify when a person is overamping and needs to rest, and when a person goes down and needs emergency medical services.
Overamping |
Overdose (OD) |
|---|---|
| Signs of overamping
Effects of the high can become more extreme with crack over-use. This happens more often when someone hasn’t slept or eaten in a while. These can include:
|
Signs of a stimulant overdose (OD)
|
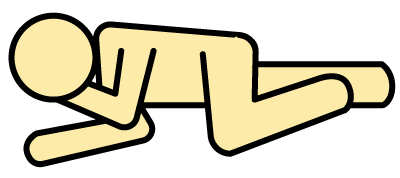
If you have to leave the person alone, put them in the
RECOVERY POSITION
Naloxone reverses an opioid overdose. There is no antidote to stimulant overdose, but the drug supply is toxic and unpredictable. Giving someone naloxone will not harm them. When in doubt, use naloxone. IT’S SAFE. Talk to your harm reduction worker about where to get support and help if you want to reduce or stop your crack use.
Thank you to the Ontario Harm Reduction Distribution Program (OHRDP); Jennifer Broad and Keith Williams from the Toronto Community Hepatitis C Program; Natalie Kaminski from the Peel Region Drug User Network; Toward the Heart BCCDC Harm Reduction Services; Street Works; Nine Circles; and HANDUP for their help in the development of the resource.
Design and layout: Pam Sloan Designs.
CATIE project leads: Rivka Kushner and Melisa Dickie.
This resource is adapted from a brochure by the Ontario Harm Reduction Distribution Program (OHRDP), 2014, which adapted an original resource by Vancouver Coastal Health, 2011.
Production of this publication has been made possible in part through financial contributions from the Ontario Ministry of Health and the Public Health Agency of Canada (PHAC).
The views expressed herein do not necessarily represent the views of our funders.