Linkage to hepatitis C care using a nurse navigator at the University of Virginia Infectious Diseases Hepatitis C Clinic
Virginia, USA
2019
With the advent of direct-acting antivirals (DAAs), hepatitis C treatment is more widely available than in the past, although linking patients to care remains challenging. This study looked at the use of a nurse navigator who provided support to link patients to hepatitis C treatment at an infectious diseases clinic. The focus of the study was linkage to care, although the study also looked at engagement across each step of the cascade or care (e.g., treatment initiation, follow-up testing). The study found that the nurse navigator was effective at engaging people in care: 76% of patients who were referred to the clinic went on to be linked to care. Even though this represents a high rate of linkage, this step remained the point in the cascade of care at which people were most likely to drop out of care.
Program description
The University of Virginia (UVA) Infectious Diseases Hepatitis C Clinic is part of the UVA hospital system. Referrals to the clinic come from other parts of the UVA hospital system, community service providers or the local health department. The clinic is staffed by a full-time nurse navigator who does linkage to care, physicians and a pharmacy-based team.
When patients are referred to the clinic, the nurse navigator contacts them by phone or letter to schedule an appointment. The nurse makes multiple attempts to reach a patient and reschedules appointments as needed. The nurse navigator also provides education and counselling over the phone and at in-person appointments.
During the appointment, the nurse ensures that any necessary paperwork for insurance coverage or patient assistance programs is complete, so that the patient is able to gain timely access to medications. Once the patient begins treatment, a pharmacy-based team is also available to provide telephone-based counselling related to the patient’s medications. If patients are lost to follow-up, the nurse continues to attempt to contact them.
Results
This observational study took place from 2014 to 2018 and focused on rates of linkage to care. Linkage to care was defined as attendance at one hepatitis C clinic appointment. The nurse navigator also collected other information about the patient’s progression through the cascade of care from referral to cure. The cascade of care phases were as follows:
- Referral to the clinic
- Linkage to care (attending an appointment)
- Medication prescribed
- Patient beginning treatment
- Patient completing treatment
- Post-treatment testing for hepatitis C
- Cure or sustained virologic response (SVR)
The nurse recorded reasons for patient drop-off at any point of the cascade.
Overall, 824 patients were included in this study and 76% (624) were successfully linked to care (i.e., attended at least one appointment). Additionally:
- 61% (502) began treatment,
- 57% (471) completed treatment
Retention of patients at each step of the cascade is depicted below.
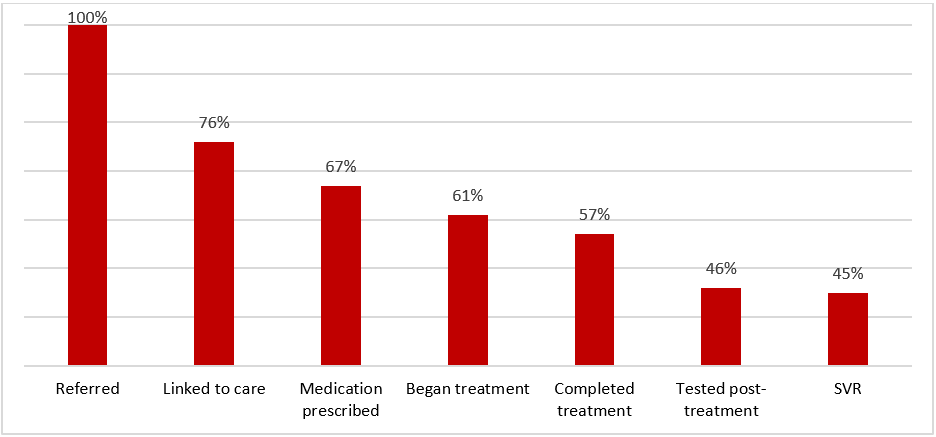
The greatest drop-off was seen in the linkage-to-care phase. The most common reasons for failure to link to care were patients not attending a scheduled appointment, inability to contact a referred patient in the first place or drop-off because of incarceration.
However, despite this drop-off, the overall rate of linkage to care was comparable to or higher than the rates reported in other studies (e.g., surveillance data reported a 17% linkage to care rate in the USA in 2016). The success of this program in linking patients to care was attributed to the use of a full-time nurse navigator who was able to actively engage patients.
What does this mean for service providers?
This study shows that use of a nurse navigator can be an effective way to support patients through the cascade of care in a clinical setting. When additional efforts are made to engage people, linkage to care tends to improve, and subsequently the rates of treatment and cure improve too. Although the biggest drop-off in the study was during linkage to care, patients who did attend appointments generally went on to begin and complete treatment. With new DAA therapies, treatment is a relatively easy process. The major hurdle now is getting people engaged in care in the first place.
Related resources
Patient Navigation - Evidence Brief
Think link: Programmatic approaches for successful linkage to HIV care - Evidence Review
Check Hep C – Evidence Brief
HepTLC – Evidence Brief
References
Sherbuk J, McManus K, Knick T et al. Disparities in hepatitis C linkage to care in the direct acting antiviral era: Findings from a referral clinic with an embedded nurse navigator model. Frontiers in Public Health. 2019;7:362.
